Ann Surg Treat Res.
2015 Jun;88(6):318-324. 10.4174/astr.2015.88.6.318.
Effect of visceral fat area on outcomes of laparoscopyassisted distal gastrectomy for gastric cancer: subgroup analysis by gender and parameters of obesity
- Affiliations
-
- 1Dong-A University College of Medicine, Busan, Korea.
- 2Department of Surgery, Dong-A University College of Medicine, Busan, Korea. mckim@donga.ac.kr
- 3Department of Radiology, Dong-A University College of Medicine, Busan, Korea.
- 4Department of Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- KMID: 1800645
- DOI: http://doi.org/10.4174/astr.2015.88.6.318
Abstract
- PURPOSE
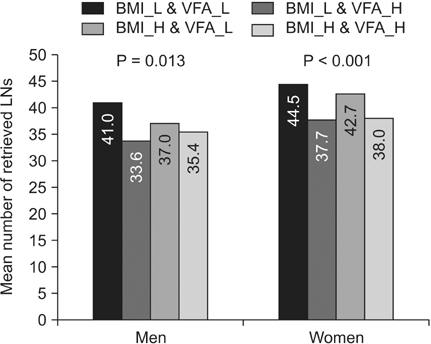
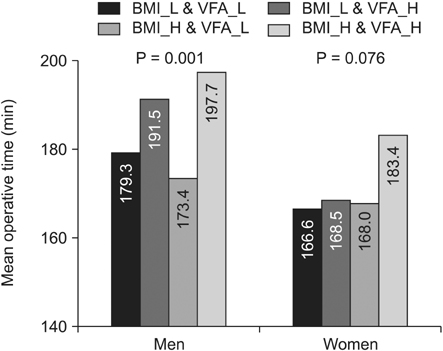
The aim of this study was to investigate the impact of the visceral fat area (VFA) of patients with gastric cancer undergoing laparoscopic surgery on operative outcomes such as number of retrieved lymph nodes (LNs) and operative time.
METHODS
We retrospectively reviewed the medical records and the CT scans of 597 patients with gastric cancer who underwent laparoscopy assisted distal gastrectomy (LADG) with partial omentectomy and LN dissection (>D1 plus beta). Patients were stratified by gender, VFA, and body mass index (BMI), and the clinicopathologic characteristics and operative outcomes were evaluated. Multiple linear regression analysis was used to assess the effects of VFA and BMI on the number of retrieved LNs and operative time in male and female patients.
RESULTS
The mean number of retrieved LNs was significantly decreased for both male and female patients with high VFA. The operative time was significantly longer for both male and female patients with high VFA. The number of retrieved LNs had a statistically significant negative correlation with VFA in both men and women, but not with BMI. The operative time had a statistically significant positive correlation with VFA in men, whereas the operative time had a statistically significant positive correlation with BMI in women.
CONCLUSION
The preoperative VFA of male patients with gastric cancer who undergo LADG may affect the number of retrieved LNs and operative time. VFA was more useful than BMI for predicting outcomes of LADG.
Keyword
MeSH Terms
Figure
Reference
-
1. van de Velde CJ, Peeters KC. The gastric cancer treatment controversy. J Clin Oncol. 2003; 21:2234–2236.2. Hyung WJ, Kim SS, Choi WH, Cheong JH, Choi SH, Kim CB, et al. Changes in treatment outcomes of gastric cancer surgery over 45 years at a single institution. Yonsei Med J. 2008; 49:409–415.3. Koeda K, Nishizuka S, Wakabayashi G. Minimally invasive surgery for gastric cancer: the future standard of care. World J Surg. 2011; 35:1469–1477.4. Hur H, Xuan Y, Ahn CW, Cho YK, Han SU. Trends and outcomes of minimally invasive surgery for gastric cancer: 750 consecutive cases in seven years at a single center. Am J Surg. 2013; 205:45–51.5. Perez Rodrigo C. Current mapping of obesity. Nutr Hosp. 2013; 28:Suppl 5. 21–31.6. Ohno T, Mochiki E, Ando H, Ogawa A, Yanai M, Toyomasu Y, et al. The benefits of laparoscopically assisted distal gastrectomy for obese patients. Surg Endosc. 2010; 24:2770–2775.7. Yamada H, Kojima K, Inokuchi M, Kawano T, Sugihara K. Effect of obesity on technical feasibility and postoperative outcomes of laparoscopy-assisted distal gastrectomy: comparison with open distal gastrectomy. J Gastrointest Surg. 2008; 12:997–1004.8. Lee JH, Paik YH, Lee JS, Ryu KW, Kim CG, Park SR, et al. Abdominal shape of gastric cancer patients influences short-term surgical outcomes. Ann Surg Oncol. 2007; 14:1288–1294.9. Shim JH, Song KY, Kim SN, Park CH. Laparoscopy-assisted distal gastrectomy for overweight patients in the Asian population. Surg Today. 2009; 39:481–486.10. Kim KH, Kim MC, Jung GJ, Kim HH. The impact of obesity on LADG for early gastric cancer. Gastric Cancer. 2006; 9:303–307.11. Yoshikawa K, Shimada M, Kurita N, Iwata T, Nishioka M, Morimoto S, et al. Visceral fat area is superior to body mass index as a predictive factor for risk with laparoscopy-assisted gastrectomy for gastric cancer. Surg Endosc. 2011; 25:3825–3830.12. Ojima T, Iwahashi M, Nakamori M, Nakamura M, Takifuji K, Katsuda M, et al. The impact of abdominal shape index of patients on laparoscopy-assisted distal gastrectomy for early gastric cancer. Langenbecks Arch Surg. 2012; 397:437–445.13. Miyaki A, Imamura K, Kobayashi R, Takami M, Matsumoto J. Impact of visceral fat on laparoscopy-assisted distal gastrectomy. Surgeon. 2013; 11:76–81.14. Sottier D, Petit JM, Guiu S, Hamza S, Benhamiche H, Hillon P, et al. Quantification of the visceral and subcutaneous fat by computed tomography: interobserver correlation of a single slice technique. Diagn Interv Imaging. 2013; 94:879–884.15. Examination Committee of Criteria for 'Obesity Disease' in Japan. Japan Society for the Study of Obesity. New criteria for 'obesity disease' in Japan. Circ J. 2002; 66:987–992.16. Ishii Y, Hasegawa H, Nishibori H, Watanabe M, Kitajima M. Impact of visceral obesity on surgical outcome after laparoscopic surgery for rectal cancer. Br J Surg. 2005; 92:1261–1262.17. Matsumoto N, Shimada M, Kurita N, Iwata T, Nishioka M, Morimoto S, et al. The role of body mass index and visceral fat area in colorectal cancer patients treated with laparoscopic-assisted surgery [abstract]. In : Society of American Gastrointestinal and Endoscopic Surgeons 2010; 2010 Apr 14-17; Los Angeles (CA): Society of American Gastrointestinal and Endoscopic Surgeons;2010.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is There any Role of Visceral Fat Area for Predicting Difficulty of Laparoscopic Gastrectomy for Gastric Cancer?
- Midterm body composition changes after open distal gastrectomy for early gastric cancer
- Larger Remaining Stomach Volume Is Associated With Better Nutrition and Muscle Preservation in Patients With Gastric Cancer Receiving Distal Gastrectomy With Gastroduodenostomy
- Association of Visceral Fat Area Measured by InBody 720 with the Results Measured by CT, DEXA and Anthropometric Measurement
- Entirely Laparoscopic Gastrectomy and Colectomy for Remnant Gastric Cancer with Gastric Outlet Obstruction and Transverse Colon Invasion