J Korean Assoc Oral Maxillofac Surg.
2014 Dec;40(6):266-271. 10.5125/jkaoms.2014.40.6.266.
Reconstruction plates used in the surgery for mandibular discontinuity defect
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Kyungpook National University School of Dentistry, Daegu, Korea. jypaeng@gmail.com
- KMID: 1799559
- DOI: http://doi.org/10.5125/jkaoms.2014.40.6.266
Abstract
OBJECTIVES
The purpose of this study was to analyze the survival rate of reconstruction plates that were used to correct mandibular discontinuity defects.
MATERIALS AND METHODS
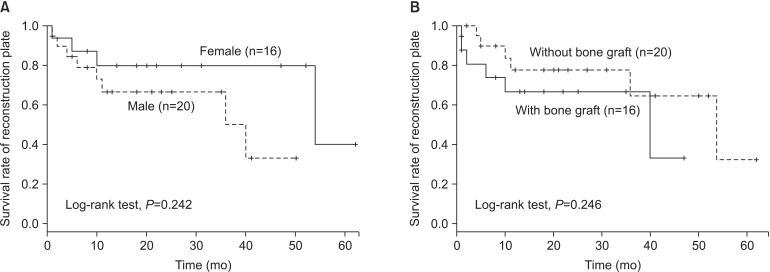
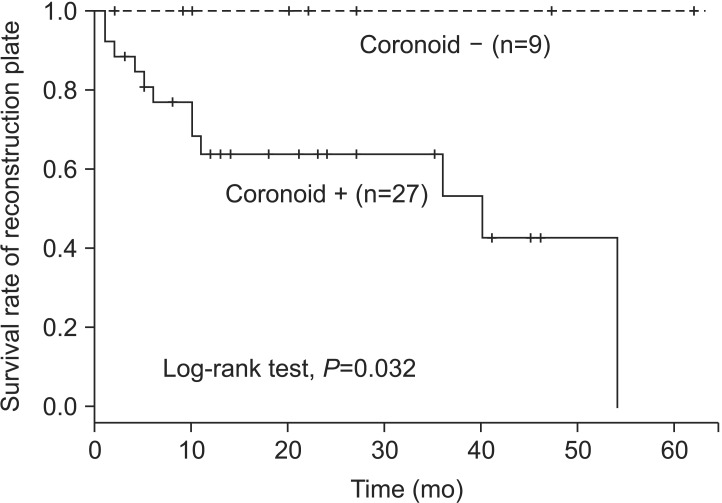
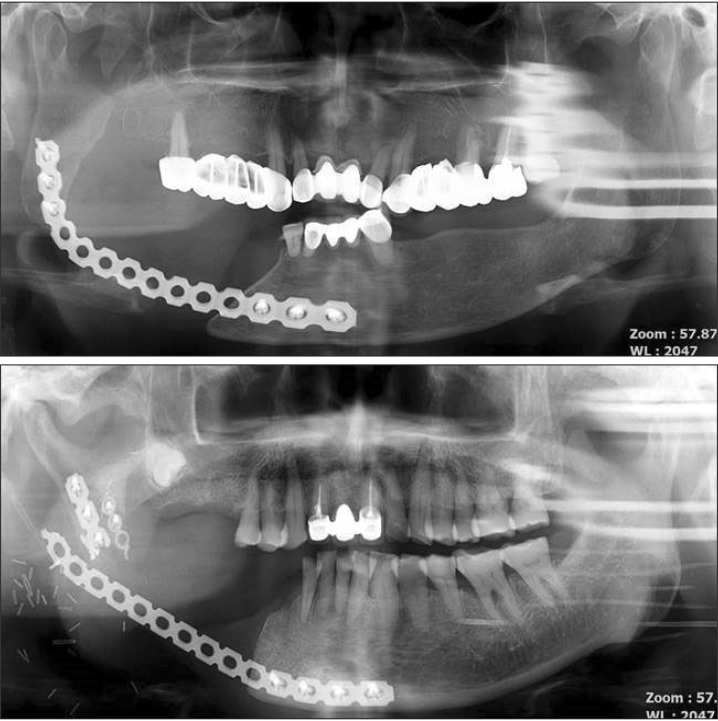
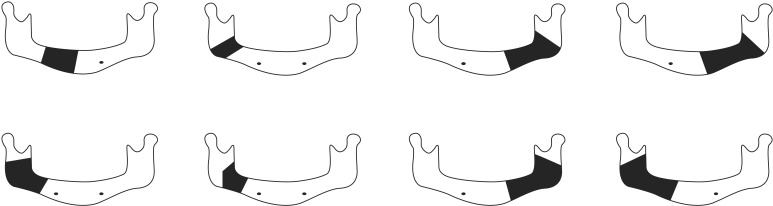
We analyzed clinical and radiological data of 36 patients. Only discontinuous mandibular defect cases were included in the study. Reconstruction plate survival rate was analyzed according to age, gender, location of defect, defect size, and whether the patient underwent a bone graft procedure, coronoidectomy, and/or postoperative radiation therapy (RT).
RESULTS
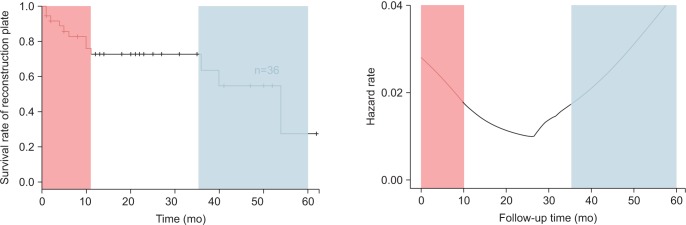
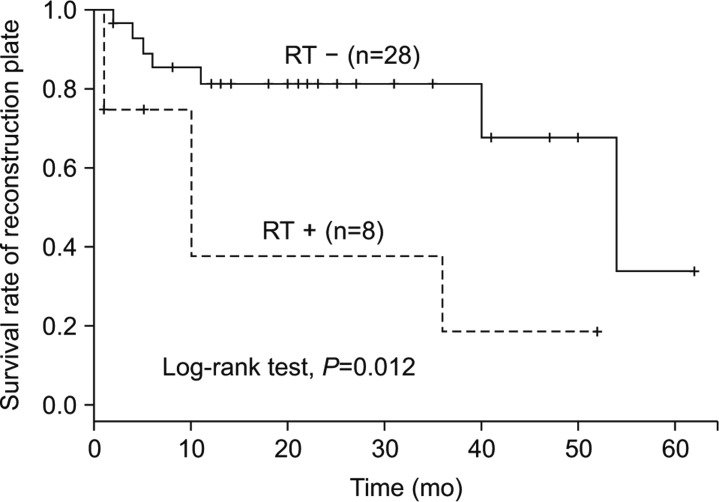
Plate-related complications developed in 8 patients, 7 of which underwent plate removal. No significant differences were found in plate survival rate according to age, gender, location of defect, defect size, or whether a bone graft procedure was performed. However, there were differences in the plate survival rate that depended on whether the patient underwent coronoidectomy or postoperative RT. In the early stages (9.25+/-5.10 months), plate fracture was the most common complication, but in the later stages (35.75+/-17.00 months), screw loosening was the most common complication.
CONCLUSION
It is important to establish the time-related risk of complications such as plate fracture or screw loosening. Coronoidectomy should be considered in most cases to prevent complications. Postoperative RT can affect the survival rate and hazard rate after a reconstruction plate is fitted.
MeSH Terms
Figure
Reference
-
1. Maurer P, Eckert AW, Kriwalsky MS, Schubert J. Scope and limitations of methods of mandibular reconstruction: a long-term follow-up. Br J Oral Maxillofac Surg. 2010; 48:100–104. PMID: 19647911.
Article2. Schmoker R, Spiessl B, Mathys R. A total mandibular plate to bridge large defects of the mandible. In : Spiessl B, Bassetti C, editors. New concepts in maxillofacial bone surgery. Berlin, New York: Springer-Verlag;1976. p. 156–159.3. Peacock ZS, Afshar S, Lukas SJ, Kaban LB. Customized repair of fractured mandibular reconstruction plates. J Oral Maxillofac Surg. 2012; 70:e563–e573. PMID: 22871312.
Article4. Knott PD, Suh JD, Nabili V, Sercarz JA, Head C, Abemayor E, et al. Evaluation of hardware-related complications in vascularized bone grafts with locking mandibular reconstruction plate fixation. Arch Otolaryngol Head Neck Surg. 2007; 133:1302–1306. PMID: 18086976.
Article5. Szypryt P, Forward D. The use and abuse of locking plates. Orthop Trauma. 2009; 23:281–290.
Article6. Klotch DW, Gal TJ, Gal RL. Assessment of plate use for mandibular reconstruction: has changing technology made a difference? Otolaryngol Head Neck Surg. 1999; 121:388–392. PMID: 10504593.
Article7. Probst FA, Mast G, Ermer M, Gutwald R, Schmelzeisen R, Pautke C, et al. MatrixMANDIBLE preformed reconstruction plates--a two-year two-institution experience in 71 patients. J Oral Maxillofac Surg. 2012; 70:e657–e666. PMID: 22868032.
Article8. Gellrich NC, Suarez-Cunqueiro MM, Otero-Cepeda XL, Schön R, Schmelzeisen R, Gutwald R. Comparative study of locking plates in mandibular reconstruction after ablative tumor surgery: THORP versus UniLOCK system. J Oral Maxillofac Surg. 2004; 62:186–193. PMID: 14762751.
Article9. Katakura A, Shibahara T, Noma H, Yoshinari M. Material analysis of AO plate fracture cases. J Oral Maxillofac Surg. 2004; 62:348–352. PMID: 15015169.
Article10. Lindqvist C, Söderholm AL, Salo A, Subasinghe J, Ylijoki S, Skutnabb K, et al. A comparative study on four screw-plate locking systems in sheep: a clinical and radiological study. Int J Oral Maxillofac Surg. 2001; 30:160–166. PMID: 11405453.
Article11. Kimura A, Nagasao T, Kaneko T, Tamaki T, Miyamoto J, Nakajima T. Adaquate fixation of plates for stability during mandibular reconstruction. J Craniomaxillofac Surg. 2006; 34:193–200. PMID: 16624567.
Article12. Arias-Gallo J, Maremonti P, González-Otero T, Gómez-García E, Burgueño-García M, Chamorro Pons M, et al. Long term results of reconstruction plates in lateral mandibular defects. Revision of nine cases. Auris Nasus Larynx. 2004; 31:57–63. PMID: 15041055.13. Nagasao T, Miyamoto J, Tamaki T, Kawana H. A comparison of stresses in implantation for grafted and plate-and-screw mandible reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:346–356. PMID: 20097102.
Article14. Faulkner MG, Hatcher DC, Hay A. A three-dimensional investigation of temporomandibular joint loading. J Biomech. 1987; 20:997–1002. PMID: 3693381.
Article15. Schöning H, Emshoff R. Primary temporary AO plate reconstruction of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 86:667–672. PMID: 9868722.
Article16. Mariani PB, Kowalski LP, Magrin J. Reconstruction of large defects postmandibulectomy for oral cancer using plates and myocutaneous flaps: a long-term follow-up. Int J Oral Maxillofac Surg. 2006; 35:427–432. PMID: 16442779.
Article17. Chepeha DB, Teknos TN, Fung K, Shargorodsky J, Sacco AG, Nussenbaum B, et al. Lateral oromandibular defect: when is it appropriate to use a bridging reconstruction plate combined with a soft tissue revascularized flap? Head Neck. 2008; 30:709–717. PMID: 18286487.
Article18. Boyd TG, Huber KM, Verbist DE, Bumpous JM, Wilhelmi BJ. Case report removal of exposed titanium reconstruction plate after mandibular reconstruction with a free fibula osteocutaneous flap with large surgical pin cutters: a case report and literature review. Eplasty. 2012; 12:e42. PMID: 22977677.19. Olascoaga A, Vilar-Compte D, Poitevin-Chacón A, Contreras-Ruiz J. Wound healing in radiated skin: pathophysiology and treatment options. Int Wound J. 2008; 5:246–257. PMID: 18494630.
Article20. Marx RE. Osteoradionecrosis: a new concept of its pathophysiology. J Oral Maxillofac Surg. 1983; 41:283–288. PMID: 6572704.
Article21. Head C, Alam D, Sercarz JA, Lee JT, Rawnsley JD, Berke GS, et al. Microvascular flap reconstruction of the mandible: a comparison of bone grafts and bridging plates for restoration of mandibular continuity. Otolaryngol Head Neck Surg. 2003; 129:48–54. PMID: 12869916.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MANDIBULAR RECONSTRUCTION WITH ALLOGENEIC MANDIBLE AND AUTOGENOUS ILIAC CNACELLOUS BONE
- Mandibular reconstruction with particulate cancellous bone and marrow
- Evaluation of Bone Resorption Rate after Nonvascularized Iliac Bone Graft for Mandibular Discontinuity Defect
- Clinical Experience in Reconstruction of the Posterior Lingual Mandibular Bony Defect
- Application Of Reconstruction Plate Using Simple Condylar Repositioning Miniplate After Segmental Resection Of Mandible