J Periodontal Implant Sci.
2013 Jun;43(3):136-140. 10.5051/jpis.2013.43.3.136.
Endodontic treatment enhances the regenerative potential of teeth with advanced periodontal disease with secondary endodontic involvement
- Affiliations
-
- 1Department of Periodontology, Pusan National University School of Dentistry, Yangsan, Korea. jrapa@pusan.ac.kr
- KMID: 1798487
- DOI: http://doi.org/10.5051/jpis.2013.43.3.136
Abstract
- PURPOSE
The aim of this study was to identify a role for endodontic intervention in enhancing the regenerative potential of the periodontal ligament when combined with periodontal treatment in seriously involved teeth with a secondary endodontic component.
METHODS
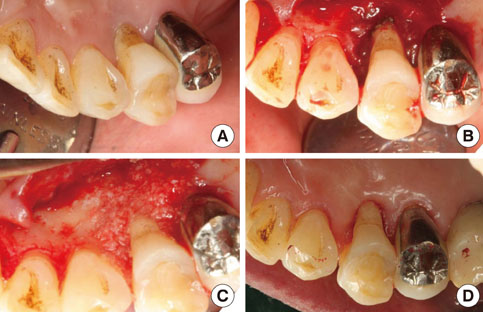
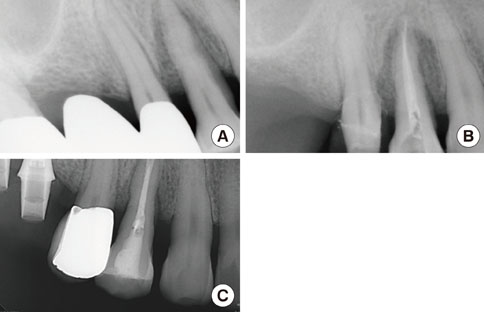
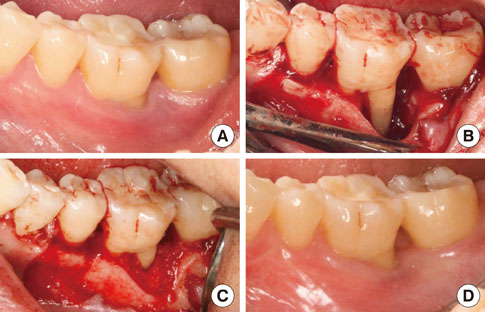
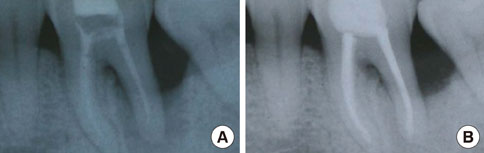
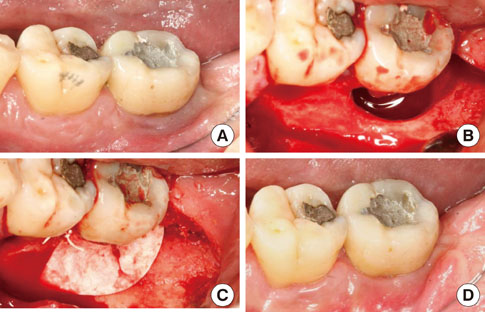
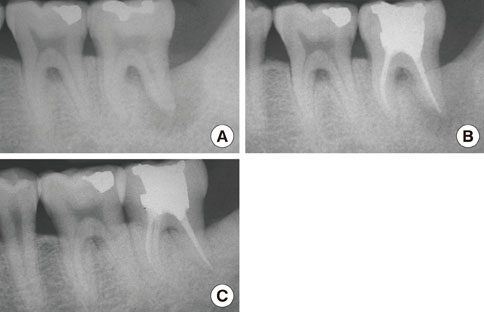
Patients who exhibited radiolucency extending to the periapical region, abnormal electric pulp testing values, and deep probing depth derived from primary periodontal disease with secondary endodontic involvement were included. Intentional root canal treatment was applied to those teeth in which the apical lesions were presumed to communicate with those of the periodontal lesion of the teeth that remained vital. In all three selected cases, regenerative periodontal therapy incorporating either bone graft or guided tissue regeneration was instituted 3 months after the endodontic intervention.
RESULTS
Remarkable enhancement in radiographic density was noticeable around the affected teeth as evidenced by changes in radiopacity. There was a significant reduction in the probing pocket depth and gain in the clinical attachment level. Chewing discomfort gradually disappeared from the commencement of the combined treatment.
CONCLUSIONS
An intentional endodontic intervention may be a worthwhile approach for the sophisticated management of teeth suffering from serious attachment loss and alveolar bone destruction with concomitant secondary endodontic involvement.
MeSH Terms
Figure
Reference
-
1. Singh P. Endo-perio dilemma: a brief review. Dent Res J (Isfahan). 2011; 8:39–47.2. Simon JH, Glick DH, Frank AL. The relationship of endodontic-periodontic lesions. J Periodontol. 1972; 43:202–208.
Article3. Zehnder M, Gold SI, Hasselgren G. Pathologic interactions in pulpal and periodontal tissues. J Clin Periodontol. 2002; 29:663–671.
Article4. Rotstein I, Simon JH. Diagnosis, prognosis and decision-making in the treatment of combined periodontal-endodontic lesions. Periodontol 2000. 2004; 34:165–203.
Article5. Langeland K, Rodrigues H, Dowden W. Periodontal disease, bacteria, and pulpal histopathology. Oral Surg Oral Med Oral Pathol. 1974; 37:257–270.
Article6. Gold SI, Moskow BS. Periodontal repair of periapical lesions: the borderland between pulpal and periodontal disease. J Clin Periodontol. 1987; 14:251–256.
Article7. Casullo DP. The integration of endodontics, periodontics and restorative dentistry in general practice. Part I. Diagnosis. Compend Contin Educ Gen Dent. 1980; 1:137–147.8. Bender IB, Seltzer S. The effect of periodontal disease on the pulp. Oral Surg Oral Med Oral Pathol. 1972; 33:458–474.
Article9. Jansson LE, Ehnevid H, Lindskog SF, Blomlof LB. Radiographic attachment in periodontitis-prone teeth with endodontic infection. J Periodontol. 1993; 64:947–953.
Article10. Blomlof L, Lindskog S, Hammarstrom L. Influence of pulpal treatments on cell and tissue reactions in the marginal periodontium. J Periodontol. 1988; 59:577–583.
Article11. Chen SY, Wang HL, Glickman GN. The influence of endodontic treatment upon periodontal wound healing. J Clin Periodontol. 1997; 24:449–456.
Article12. Bergenholtz G, Lekholm U, Liljenberg B, Lindhe J. Morphometric analysis of chronic inflammatory periapical lesions in root-filled teeth. Oral Surg Oral Med Oral Pathol. 1983; 55:295–301.
Article13. Meng HX. Periodontic-endodontic lesions. Ann Periodontol. 1999; 4:84–90.
Article14. Oh SL, Fouad AF, Park SH. Treatment strategy for guided tissue regeneration in combined endodontic-periodontal lesions: case report and review. J Endod. 2009; 35:1331–1336.
Article15. Tseng CC, Harn WM, Chen YH, Huang CC, Yuan K, Huang PH. A new approach to the treatment of true-combined endodontic-periodontic lesions by the guided tissue regeneration technique. J Endod. 1996; 22:693–696.
Article16. Rankow HJ, Krasner PR. Endodontic applications of guided tissue regeneration in endodontic surgery. J Endod. 1996; 22:34–43.
Article17. Britain SK, Arx Tv, Schenk RK, Buser D, Nummikoski P, Cochran DL. The use of guided tissue regeneration principles in endodontic surgery for induced chronic periodontic-endodontic lesions: a clinical, radiographic, and histologic evaluation. J Periodontol. 2005; 76:450–460.
Article18. Camelo MC, Nevins ML, Nevins M. Treatment of Class II furcations with autogenous bone grafts and e-PTFE membranes. Int J Periodontics Restorative Dent. 2000; 20:233–243.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A review of the regenerative endodontic treatment procedure
- Diagnosis and treatment of teeth with primary endodontic lesions mimicking periodontal disease: three cases with long-term follow ups
- Management of failed periodontal surgical intervention for a furcal lesion with a nonsurgical endodontic approach
- Guided tissue regeneration therapy after root canal therapy for long standing periodontal-endodontic combined lesion in the mandibular anterior area: case report
- Prevalence of referral reasons and clinical symptoms for endodontic referrals