J Periodontal Implant Sci.
2013 Jun;43(3):130-135. 10.5051/jpis.2013.43.3.130.
Evaluation of tensile strength of surgical synthetic absorbable suture materials: an in vitro study
- Affiliations
-
- 1Department of Periodontology, AECS Maaruti College of Dental Sciences and Research Centre, Bangalore, India. drsujeetperio@gmail.com
- KMID: 1798486
- DOI: http://doi.org/10.5051/jpis.2013.43.3.130
Abstract
- PURPOSE
The purpose of this study was to evaluate the tensile strength of surgical synthetic absorbable sutures over a period of 14 days under simulated oral conditions.
METHODS
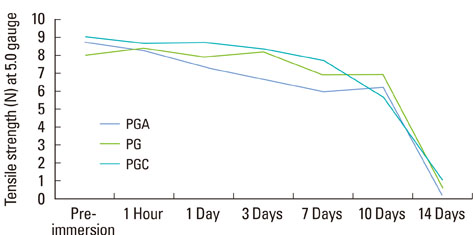
Three suture materials (polyglycolic acid [PGA], polyglactin [PG] 910, and poly (glycolide-co-small je, Ukrainian-caprolactone) [PGC]) were used in 4-0 and 5-0 gauges. 210 suture samples (35 of each material and gauge) were used. All of the samples were tested preimmersion and 1 hour and 1, 3, 7, 10, and 14 days postimmersion. The tensile strength of each suture material and gauge was assessed. The point of breakage and the resorption pattern of the sutures were also assessed.
RESULTS
During the first 24 hours of immersion, all 4-0 and 5-0 samples of PGA, PG 910, and PGC maintained their initial tensile strength. At baseline (preimmersion), there was a statistically significant (P<0.001) difference in the tensile strengths between the 4-0 and 5-0 gauge of PGA, PG 910, and PGC. PGA 4-0 showed the highest tensile strength until day 10. At 7 days, all the 4-0 sutures of the three materials had maintained their tensile strength with PGA 4-0 having significantly greater (P=0.003) tensile strength compared to PG.
CONCLUSIONS
4-0 sutures are stronger and have greater tensile strength than 5-0 sutures. The PGA 4-0 suture showed the highest tensile strength at the end of day 10.
Keyword
MeSH Terms
Figure
Reference
-
1. Parell GJ, Becker GD. Comparison of absorbable with nonabsorbable sutures in closure of facial skin wounds. Arch Facial Plast Surg. 2003; 5:488–490.
Article2. Pillai CK, Sharma CP. Review paper: absorbable polymeric surgical sutures: chemistry, production, properties, biodegradability, and performance. J Biomater Appl. 2010; 25:291–366.
Article3. Wikesjo UM, Nilveus RE, Selvig KA. Significance of early healing events on periodontal repair: a review. J Periodontol. 1992; 63:158–165.
Article4. Vasanthan A, Satheesh K, Hoopes W, Lucaci P, Williams K, Rapley J. Comparing suture strengths for clinical applications: a novel in vitro study. J Periodontol. 2009; 80:618–624.
Article5. Yaltirik M, Dedeoglu K, Bilgic B, Koray M, Ersev H, Issever H, et al. Comparison of four different suture materials in soft tissues of rats. Oral Dis. 2003; 9:284–286.
Article6. Karaca E, Hockenberger AS, Yildiz H. Investigating changes in mechanical properties and tissue reaction of silk, polyester, polyamide, and polypropylene sutures in vivo. Text Res J. 2005; 75:297–303.
Article7. Moore RL, Hill M. Suturing techniques for periodontal plastic surgery. Periodontol 2000. 1996; 11:103–111.
Article8. Ferguson RE Jr, Schuler K, Thornton BP, Vasconez HC, Rinker B. The effect of saliva and oral intake on the tensile properties of sutures: an experimental study. Ann Plast Surg. 2007; 58:268–272.
Article9. Nary Filho H, Matsumoto MA, Batista AC, Lopes LC, de Goes FC, Consolaro A. Comparative study of tissue response to polyglecaprone 25, polyglactin 910 and polytetrafluorethylene suture materials in rats. Braz Dent J. 2002; 13:86–91.
Article10. van Heerden J. Comparison of inflammatory response to polyglytone 6211 and polyglecaprone 25 in a rat model. S Afr Med J. 2005; 95:972–974.11. Huang TW, Cheng PW, Chan YH, Wang CT, Fang KM, Young TH. Clinical and biomechanical analyses to select a suture material for uvulopalatopharyngeal surgery. Otolaryngol Head Neck Surg. 2010; 143:655–661.
Article12. Moser JB, Lautenschlager EP, Horbal BJ. Mechanical properties of polyglycolic acid sutures in oral surgery. J Dent Res. 1974; 53:804–808.
Article13. Brown RP. Knotting technique and suture materials. Br J Surg. 1992; 79:399–400.
Article14. Zoller GO, Zentner A. Initial attachment of human gingival fibroblast-like cells in vitro to titanium surfaces pretreated with saliva and serum. Clin Oral Implants Res. 1996; 7:311–315.15. Chu CC, Moncrief G. An in vitro evaluation of the stability of mechanical properties of surgical suture materials in various pH conditions. Ann Surg. 1983; 198:223–228.
Article16. Kim JC, Lee YK, Lim BS, Rhee SH, Yang HC. Comparison of tensile and knot security properties of surgical sutures. J Mater Sci Mater Med. 2007; 18:2363–2369.
Article17. Pavan A, Bosio M, Longo T. A comparative study of poly (glycolic acid) and catgut as suture materials: histomorphology and mechanical properties. J Biomed Mater Res. 1979; 13:477–496.
Article18. von Fraunhofer JA, Storey RJ, Masterson BJ. Tensile properties of suture materials. Biomaterials. 1988; 9:324–327.
Article19. Shetty PC, Dicksheet S, Scalea TM. Emergency department repair of hand lacerations using absorbable vicryl sutures. J Emerg Med. 1997; 15:673–674.
Article20. Tiyek I, Gemci R, Turkoglu S. Comparison of physical properties of sutures in medical liquids. Int J Phys Sci. 2011; 6:2158–2168.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparative Study of Tensile Strength in Vitro and Histologic Reaction on Rabbits between TRISORB Suture Materials and Traditional Suture Materials ( Dexon , Vicryl , Medifit )
- Comparative Study of Subcutaneous Buried Suture Materials in Rabbits
- A Comparative Study of the Use of 9-0 PDS and 9-0 Ethilon in Microvascular Anastomosis
- Comparative Study of Absorbable Suture Material and Nonabsorbable Suture Material in Micro - Vascular Anastomosis: An Experimental Study on 1 mm Diameter Arterial Anastomosis in the Garotid Artery of Rat
- Comparative Study of Tissue Response of Various Suture Materials in Rats