J Korean Foot Ankle Soc.
2015 Jun;19(2):69-72. 10.14193/jkfas.2015.19.2.69.
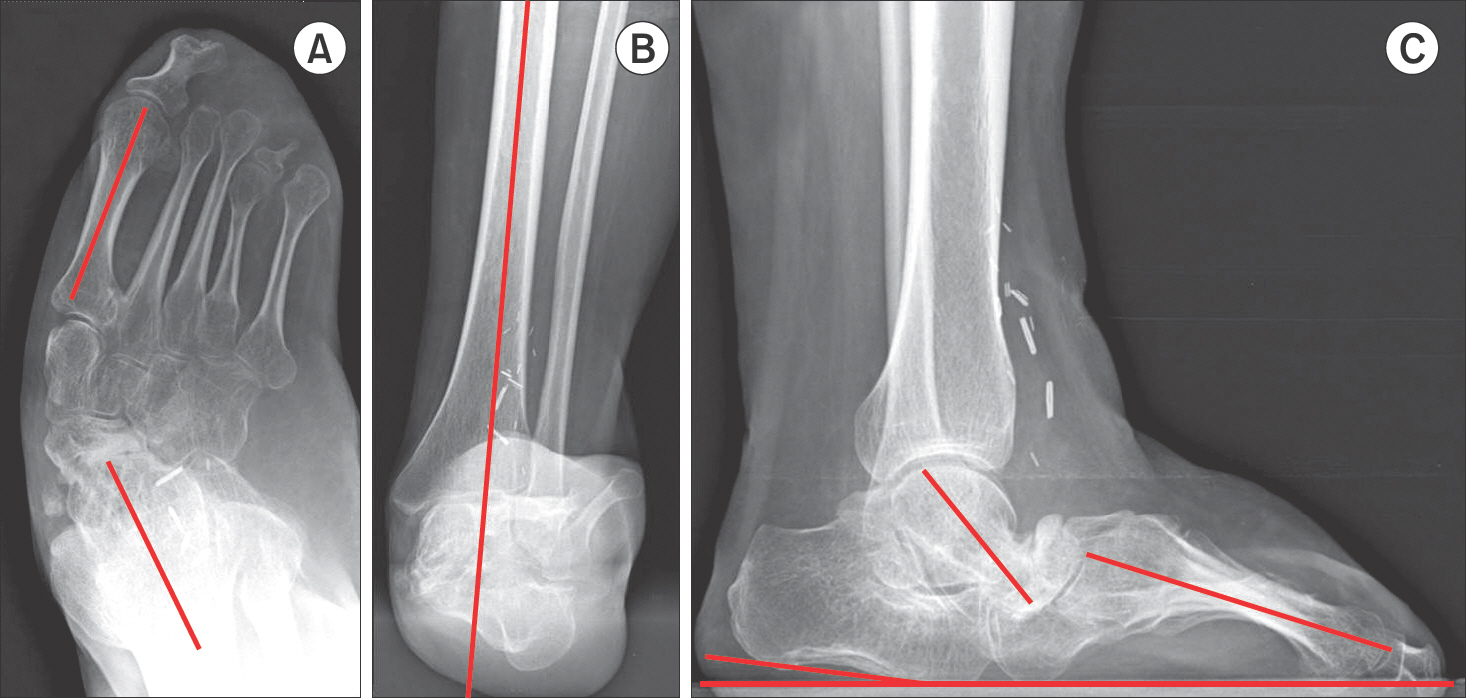
Isolated Talonavicular Arthrodesis as an Option for Severe Rocker Bottom Foot Deformity: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Inje University Ilsan Paik Hospital, Goyang, Korea. sjs0506@paik.ac.kr
- 2Department of Surgery, Howard University College of Medicine, Washington, DC, USA.
- KMID: 1794886
- DOI: http://doi.org/10.14193/jkfas.2015.19.2.69
Abstract
- We report on a case of post-burn contracture and right foot deformity in a 37-year-old female who underwent two surgical interventions at the age of seven years. The patient remained well without any associated problems until she presented to our hospital at the age of 37 years with severe pain and right foot deformity. A few treatment modalities have been reported, and amputation has been suggested as the best approach. However, our patient was treated with a talonavicular arthrodesis and a soft tissue procedure, which resulted in a stable, plantigrade, and pain-free foot with an unsupported, bipedal gait.
Keyword
Figure
Reference
-
1.Thelen S., Rütt J., Wild M., Lögters T., Windolf J., Koebke J. The influence of talonavicular versus double arthrodesis on load dependent motion of the midtarsal joint. Arch Orthop Trauma Surg. 2010. 130:47–53.
Article2.Kiesau CD., Larose CR., Glisson RR., Easley ME., Deorio JK. Talonavicular joint fixation using augmenting naviculocalcaneal screw in modified double hindfoot arthrodesis. Foot Ankle Int. 2011. 32:244–9.
Article3.Swaroop VT., Wenger DR., Mubarak SJ. Talonavicular fusion for dorsal subluxation of the navicular in resistant clubfoot. Clin Orthop Relat Res. 2009. 467:1314–8.
Article4.Popelka S., Hromádka R., Vavrík P., Stursa P., Pokorný D., Jahoda D, et al. Isolated talonavicular arthrodesis in patients with rheumatoid arthritis of the foot and tibialis posterior tendon dysfunction. BMC Musculoskelet Disord. 2010. 11:38.
Article5.Ljung P., Kaij J., Knutson K., Pettersson H., Rydholm U. Talonavicular arthrodesis in the rheumatoid foot. Foot Ankle. 1992. 13:313–6.
Article6.Philippot R., Wegrzyn J., Besse JL. Arthrodesis of the subtalar and talonavicular joints through a medial surgical approach: a series of 15 cases. Arch Orthop Trauma Surg. 2010. 130:599–603.
Article7.Carmichael KD., Maxwell SC., Calhoun JH. Recurrence rates of burn contracture ankle equinus and other foot deformities in children treated with Ilizarov fixation. J Pediatr Orthop. 2005. 25:523–8.
Article8.Saghieh S., El Bitar Y., Berjawi G., Harfouche B., Atiyeh B. Distraction histogenesis in ankle burn deformities. J Burn Care Res. 2011. 32:160–5.
Article9.Faraj AA. Talonavicular joint arthrodesis for paralytic post poliomyelitis forefoot instability. J Foot Ankle Surg. 1996. 35:166–8.
Article10.Fortin PT. Posterior tibial tendon insufficiency. Isolated fusion of the talonavicular joint. Foot Ankle Clin. 2001. 6:137–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Talonavicular Subluxation Accompanied by Calcaneal Malunion: A Case Report
- Interpositional Arthroplasty Using Tibialis Anterior Tendon for Talonavicular Arthritis after Ankle Arthrodesis: A Case Report
- Surgical Treatment of Muller-Weiss Disease: A Case Report
- Prosthetic Shoes for the Solid Ankles: Modification of the Solid-ankle Cushion-heel Foot
- The Surgical Outcome of Tibiotalocalcaneal Arthrodesis Using a Retrograde Intramedullary Nail