Radiofrequency Ablation to Treat Loco-Regional Recurrence of Well-Differentiated Thyroid Carcinoma
- Affiliations
-
- 1Department of Radiology, Chung-Ang University Hospital, Seoul 156-755, Korea.
- 2Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea. sljung1@catholic.ac.kr
- 3Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- 4Department of Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- 5Department of Otolaryngology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- 6Department of Clinical Pathology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- KMID: 1794655
- DOI: http://doi.org/10.3348/kjr.2014.15.6.817
Abstract
OBJECTIVE
To evaluate the efficacy of radiofrequency ablation (RFA) in the treatment of loco-regional, recurrent, and well-differentiated thyroid carcinoma.
MATERIALS AND METHODS
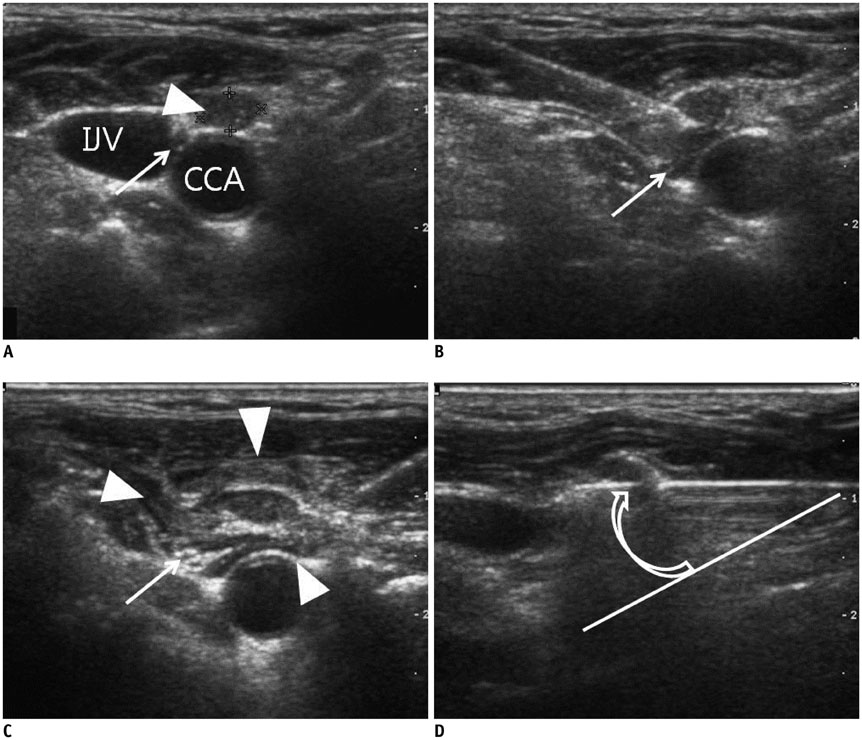
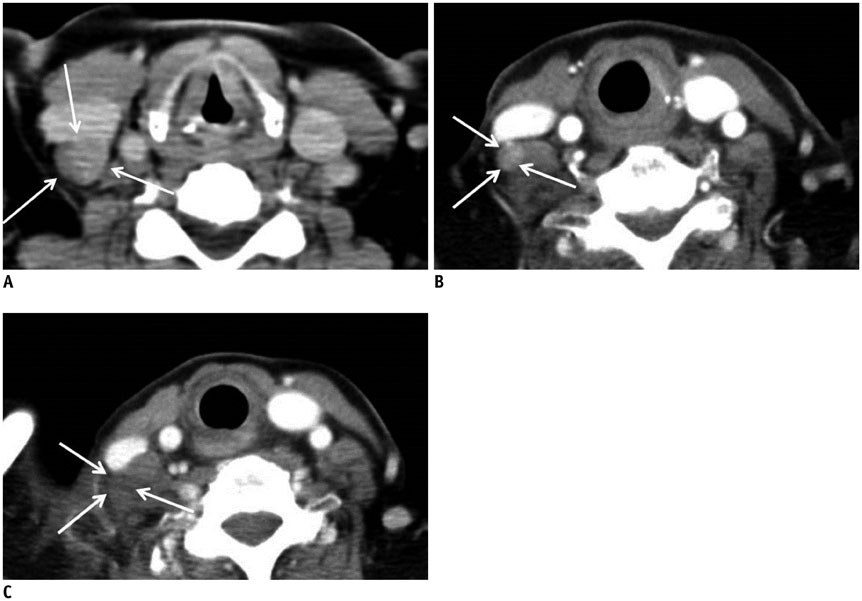
Thirty-five recurrent well-differentiated thyroid carcinomas (RTC) in 32 patients were treated with RFA, between March 2008 and October 2011. RTCs were detected by regular follow-up ultrasound and confirmed by biopsy. All patients had fewer than 3 RTCs in the neck and were at high surgical risk or refused to undergo repeated surgery. Average number of RFA sessions were 1.3 (range 1-3). Post-RFA biopsy and ultrasound were performed. The mean follow-up period was 30 months. Pre- and post-RFA serum thyroglobulin values were evaluated.
RESULTS
Thirty-one patients with 33 RTCs were treated with RFA only, whereas 1 patient with 2 RTCs was treated with RFA followed by surgery. At the last follow-up ultrasound, 31 (94%) of the 33 RTCs treated with RFA alone completely disappeared and the remaining 2 (6%) RTCs showed decreased volume. The largest diameter and volume of the 33 RTCs were markedly decreased by 93.2% (from 8.1 +/- 3.4 mm to 0.6 +/- 1.8 mm, p < 0.001) and 96.4% (from 173.9 +/- 198.7 mm3 to 6.2 +/- 27.9 mm3, p < 0.001), respectively. Twenty of the 21 RTCs evaluated with post-RFA biopsies (95%) were negative for malignancy. One (5%) showed remaining tumor that was removed surgically. The serum thyroglobulin was decreased in 19 of 26 patients (73%). Voice change developed immediately after RFA in 6 patients (19%) and was spontaneously recovered in 5 patients (83%).
CONCLUSION
Radiofrequency ablation can be effective in treating loco-regional, recurrent, and well-differentiated thyroid carcinoma in patients at high surgical risk.
MeSH Terms
Figure
Cited by 5 articles
-
Ultrasound-Guided Percutaneous Ethanol Ablation for the Management of Recurrent Thyroid Cancer: Evaluation of Efficacy and Impact on Disease Course
Santiago Tofé, Iñaki Argüelles, Guillermo Serra, Honorato García, Antonia Barcelo, Vicente Pereg
Int J Thyroidol. 2020;13(2):128-141. doi: 10.11106/ijt.2020.13.2.128.Radiofrequency versus Ethanol Ablation for Treating Predominantly Cystic Thyroid Nodules: A Randomized Clinical Trial
Jung Hwan Baek, Eun Ju Ha, Young Jun Choi, Jin Yong Sung, Jae Kyun Kim, Young Kee Shong
Korean J Radiol. 2015;16(6):1332-1340. doi: 10.3348/kjr.2015.16.6.1332.2017 Thyroid Radiofrequency Ablation Guideline: Korean Society of Thyroid Radiology
Ji-hoon Kim, Jung Hwan Baek, Hyun Kyung Lim, Hye Shin Ahn, Seon Mi Baek, Yoon Jung Choi, Young Jun Choi, Sae Rom Chung, Eun Ju Ha, Soo Yeon Hahn, So Lyung Jung, Dae Sik Kim, Soo Jin Kim, Yeo Koon Kim, Chang Yoon Lee, Jeong Hyun Lee, Kwang Hwi Lee, Young Hen Lee, Jeong Seon Park, Hyesun Park, Jung Hee Shin, Chong Hyun Suh, Jin Yong Sung, Jung Suk Sim, Inyoung Youn, Miyoung Choi, Dong Gyu Na,
Korean J Radiol. 2018;19(4):632-655. doi: 10.3348/kjr.2018.19.4.632.Ethanol Ablation of the Thyroid Nodules: 2018 Consensus Statement by the Korean Society of Thyroid Radiology
Soo Yeon Hahn, Jung Hee Shin, Dong Gyu Na, Eun Joo Ha, Hye Shin Ahn, Hyun Kyung Lim, Jeong Hyun Lee, Jeong Seon Park, Ji-hoon Kim, Jin Yong Sung, Joon Hyung Lee, Jung Hwan Baek, Jung Hyun Yoon, Jung Suk Sim, Kwang Hwi Lee, Seon Mi Baek, So Lyung Jung, Yeo Koon Kim, Yoon Jung Choi, ,
Korean J Radiol. 2019;20(4):609-620. doi: 10.3348/kjr.2018.0696.Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part III. Management of Advanced Differentiated Thyroid Cancers - Chapter 1-2. Locally Recurred/Persistent Thyroid Cancer Management Strategies 2024
Ho-Ryun Won, Min Kyoung Lee, Ho-Cheol Kang, Bon Seok Koo, Hyungju Kwon, Sun Wook Kim, Won Woong Kim, Jung-Han Kim, Young Joo Park, Jun-Ook Park, Young Shin Song, Seung Hoon Woo, Chang Hwan Ryu, Eun Kyung Lee, Joon-Hyop Lee, Ji Ye Lee, Cho Rok Lee, Dong-Jun Lim, Jae-Yol Lim, Yun Jae Chung, Kyorim Back, Dong Gyu Na
Int J Thyroidol. 2024;17(1):147-152. doi: 10.11106/ijt.2024.17.1.147.
Reference
-
1. Kumar V, Abbas AK, Aster JC. Robbins and Cotran Pathologic Basis of Disease. 9th ed. Philadelphia: Saunders;2014. p. 1073–1139.2. Gilliland FD, Hunt WC, Morris DM, Key CR. Prognostic factors for thyroid carcinoma. A population-based study of 15,698 cases from the Surveillance, Epidemiology and End Results (SEER) program 1973-1991. Cancer. 1997; 79:564–573.3. Dupuy DE, Monchik JM. Radiofrequency ablation of recurrent thyroid cancer. In : Ellis LM, Curley SA, Tanabe KK, editors. Radiofrequency Ablation for Cancer: Current indications, techniques, and outcomes. New York: Springer-Verlag;2003. p. 213–223.4. Loh KC, Greenspan FS, Gee L, Miller TR, Yeo PP. Pathological tumor-node-metastasis (pTNM) staging for papillary and follicular thyroid carcinomas: a retrospective analysis of 700 patients. J Clin Endocrinol Metab. 1997; 82:3553–3562.5. Samaan NA, Schultz PN, Hickey RC, Goepfert H, Haynie TP, Johnston DA, et al. The results of various modalities of treatment of well differentiated thyroid carcinomas: a retrospective review of 1599 patients. J Clin Endocrinol Metab. 1992; 75:714–720.6. Mazzaferri EL, Young RL. Papillary thyroid carcinoma: a 10 year follow-up report of the impact of therapy in 576 patients. Am J Med. 1981; 70:511–518.7. Esnaola NF, Cantor SB, Sherman SI, Lee JE, Evans DB. Optimal treatment strategy in patients with papillary thyroid cancer: a decision analysis. Surgery. 2001; 130:921–930.8. Dupuy DE, Monchik JM, Decrea C, Pisharodi L. Radiofrequency ablation of regional recurrence from well-differentiated thyroid malignancy. Surgery. 2001; 130:971–977.9. Monchik JM, Donatini G, Iannuccilli J, Dupuy DE. Radiofrequency ablation and percutaneous ethanol injection treatment for recurrent local and distant well-differentiated thyroid carcinoma. Ann Surg. 2006; 244:296–304.10. Baek JH, Kim YS, Sung JY, Choi H, Lee JH. Locoregional control of metastatic well-differentiated thyroid cancer by ultrasound-guided radiofrequency ablation. AJR Am J Roentgenol. 2011; 197:W331–W336.11. Shin JE, Baek JH, Lee JH. Radiofrequency and ethanol ablation for the treatment of recurrent thyroid cancers: current status and challenges. Curr Opin Oncol. 2013; 25:14–19.12. Park KW, Shin JH, Han BK, Ko EY, Chung JH. Inoperable symptomatic recurrent thyroid cancers: preliminary result of radiofrequency ablation. Ann Surg Oncol. 2011; 18:2564–2568.13. Lewis BD, Hay ID, Charboneau JW, McIver B, Reading CC, Goellner JR. Percutaneous ethanol injection for treatment of cervical lymph node metastases in patients with papillary thyroid carcinoma. AJR Am J Roentgenol. 2002; 178:699–704.14. Na DG, Lee JH, Jung SL, Kim JH, Sung JY, Shin JH, et al. Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol. 2012; 13:117–125.15. Baek JH, Lee JH, Sung JY, Bae JI, Kim KT, Sim J, et al. Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology. 2012; 262:335–342.16. Goldberg SN, Charboneau JW, Dodd GD 3rd, Dupuy DE, Gervais DA, Gillams AR, et al. Image-guided tumor ablation: proposal for standardization of terms and reporting criteria. Radiology. 2003; 228:335–345.17. Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S199–S202.18. Papini E, Bizzarri G, Bianchini A, Valle D, Misischi I, Guglielmi R, et al. Percutaneous ultrasound-guided laser ablation is effective for treating selected nodal metastases in papillary thyroid cancer. J Clin Endocrinol Metab. 2013; 98:E92–E97.19. Mauri G, Cova L, Tondolo T, Ierace T, Baroli A, Di Mauro E, et al. Percutaneous laser ablation of metastatic lymph nodes in the neck from papillary thyroid carcinoma: preliminary results. J Clin Endocrinol Metab. 2013; 98:E1203–E1207.20. Pacella CM, Bizzarri G, Guglielmi R, Anelli V, Bianchini A, Crescenzi A, et al. Thyroid tissue: US-guided percutaneous interstitial laser ablation-a feasibility study. Radiology. 2000; 217:673–677.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- RE: Papillary Thyroid Carcinoma Treated with Radiofrequency Ablation in a Patient with Hypertrophic Cardiomyopathy: A Case Report
- Papillary Thyroid Carcinoma Treated with Radiofrequency Ablation in a Patient with Hypertrophic Cardiomyopathy: A Case Report
- Radiofrequency ablation of recurrent thyroid cancers: anatomy-based management
- Effective and Safe Application of Radiofrequency Ablation for Benign Thyroid Nodules
- Response: Inquiries Regarding “Delayed Cancer Diagnosis in Thyroid Nodules Initially Treated as Benign With Radiofrequency Ablation: Ultrasound Characteristics and Predictors for Cancer”