J Korean Med Sci.
2010 Apr;25(4):651-655. 10.3346/jkms.2010.25.4.651.
Prophylactic Hypogastric Artery Ballooning in a Patient with Complete Placenta Previa and Increta
- Affiliations
-
- 1Department of Obstetrics and Gynecology, College of Medicine, Korea University, Seoul, Korea. mjohmd@korea.ac.kr
- 2Department of Radiology, College of Medicine, Korea University, Seoul, Korea.
- KMID: 1792943
- DOI: http://doi.org/10.3346/jkms.2010.25.4.651
Abstract
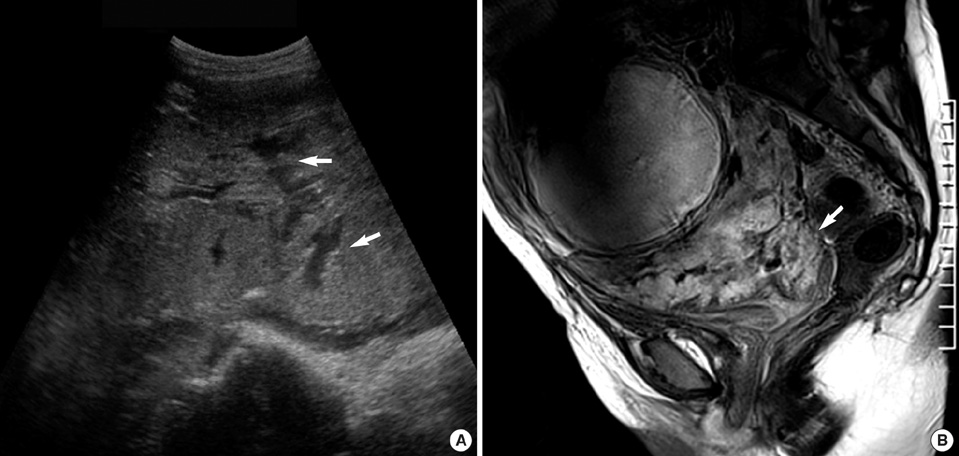
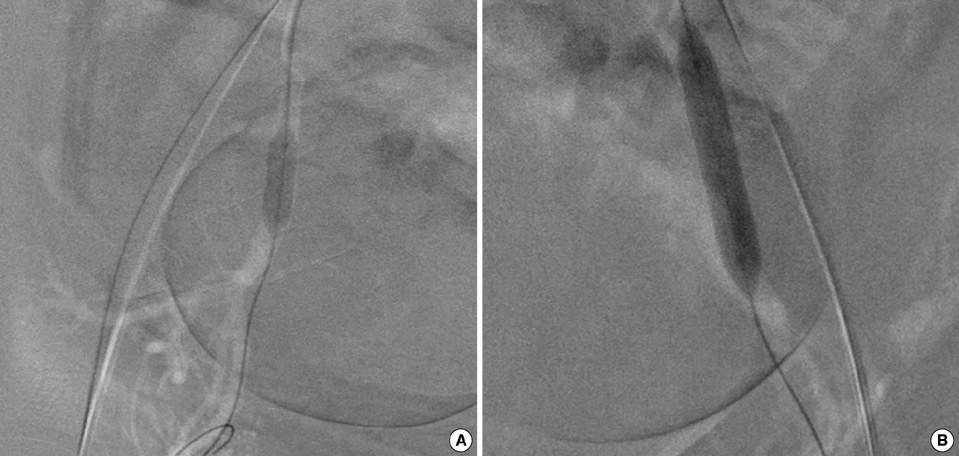
- Abnormal attachment of the placenta (Placenta accreta, increta, and percreta) is an uncommon but potentially lethal cause of maternal mortality from massive postpartum hemorrhage. A 33-yr-old woman, who had been diagnosed with a placenta previa, was referred at 30 weeks gestation. On ultrasound, a complete type of placenta previa and multiple intraplacental lacunae, suggestive of placenta accreta, were noted. For further evaluation of the placenta, pelvis MRI was performed and revealed findings suspicious of a placenta increta. An elective cesarean delivery and subsequent hysterectomy were planned for the patient at 38 weeks gestation. On the day of delivery, endovascular catheters for balloon occlusion were placed within the hypogastric arteries, prior to the cesarean section. In the operating room, immediately after the delivery of the baby, bilateral hypogastric arteries were occluded by inflation of the balloons in the catheters previously placed within. With the placenta retained within the uterus, a total hysterectomy was performed in the usual fashion. The occluding balloons were deflated after closure of the vaginal cuff with hemostasis. The patient had stable vital signs and normal laboratory findings during the recovery period; she was discharged six days after delivery without complications. The final pathology confirmed a placenta increta.
MeSH Terms
Figure
Cited by 1 articles
-
Recent Update of Embolization of Postpartum Hemorrhage
Chengshi Chen, Sang Min Lee, Jong Woo Kim, Ji Hoon Shin
Korean J Radiol. 2018;19(4):585-596. doi: 10.3348/kjr.2018.19.4.585.
Reference
-
1. Lax A, Prince MR, Mennitt KW, Schwebach JR, Budorick NE. The value of specific MRI features in the evaluation of suspected placental invasion. Magn Reson Imaging. 2007. 25:87–93.
Article2. Bodner LJ, Nosher JL, Gribbin C, Siegel RL, Beale S, Scorza W. Balloon-assisted occlusion of the internal iliac arteries in patients with placenta accreta/percreta. Cardiovasc Intervent Radiol. 2006. 29:354–361.
Article3. Berg CJ, Atrash HK, Koonin LM, Tucker M. Pregnancy-related mortality in the United States, 1987-1990. Obstet Gynecol. 1996. 88:161–167.
Article4. Stanco LM, Schrimmer DB, Paul RH, Mishell DR Jr. Emergency peripartum hysterectomy and associated risk factors. Am J Obstet Gynecol. 1993. 168:879–883.
Article5. Levine AB, Kuhlman K, Bonn J. Placenta accreta: comparison of cases managed with and without pelvic artery balloon catheters. J Matern Fetal Med. 1999. 8:173–176.
Article6. Alkazaleh F, Geary M, Kingdom J, Kachura JR, Windrim R. Elective non-removal of the placenta and prophylactic uterine artery embolization postpartum as a diagnostic imaging approach for the management of placenta percreta: a case report. J Obstet Gynaecol Can. 2004. 26:743–746.
Article7. Alvarez M, Lockwood CJ, Ghidini A, Dottino P, Mitty HA, Berkowitz RL. Prophylactic and emergent arterial catheterization for selective embolization in obstetric hemorrhage. Am J Perinatol. 1992. 9:441–444.
Article8. Kidney DD, Nguyen AM, Ahdoot D, Bickmore D, Deutsch LS, Majors C. Prophylactic perioperative hypogastric artery balloon occlusion in abnormal placentation. AJR Am J Roentgenol. 2001. 176:1521–1524.
Article9. Weeks SM, Stroud TH, Sandhu J, Mauro MA, Jaques PF. Temporary balloon occlusion of the internal iliac arteries for control of hemorrhage during cesarean hysterectomy in a patient with placenta previa and placenta increta. J Vasc Interv Radiol. 2000. 11:622–624.
Article10. Greenberg JI, Suliman A, Iranpour P, Angle N. Prophylactic balloon occlusion of the internal iliac arteries to treat abnormal placentation: a cautionary case. Am J Obstet Gynecol. 2007. 197:470.el–470.e4.
Article11. Dubois J, Garel L, Grignon A, Lemay M, Leduc L. Placenta percreta: balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. Am J Obstet Gynecol. 1997. 176:723–726.
Article12. Brent RL. Utilization of developmental basic science principles in the evaluation of reproductive risks from pre- and postconception environmental radiation exposures. Teratology. 1999. 59:182–204.
Article13. National Radiological Protection Board. Board statement on diagnostic medical exposures to ionizing radiation during pregnancy. Documents of the NRPB 4(4). 1993. London: HMSO.14. Vedantham S, Goodwin SC, McLucas B, Mohr G. Uterine artery embolization: an underused method of controlling pelvic hemorrhage. Am J Obstet Gynecol. 1997. 176:938–948.
Article15. Read JA, Cotton DB, Miller FC. Placenta accreta: changing clinical aspects and outcome. Obstet Gynecol. 1980. 56:31–34.16. Pelosi M, Langer A, Hung C. Prophylactic internal iliac artery ligation at cesarean hysterectomy. Am J Obstet Gynecol. 1975. 121:394–398.
Article17. Nizard J, Barrinque L, Frydman R, Fernandez H. Fertility and pregnancy outcomes following hypogastric artery ligation for severe postpartum haemorrhage. Hum Reprod. 2003. 18:844–848.
Article18. Sziller I, Hupuczi P, Papp Z. Hypogastric artery ligation for severe hemorrhage in obstetric patients. J Perinat Med. 2007. 35:187–192.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Conservative management of placenta increta treated with selective uterine artery embolization: Review of two cases
- A Case of Placenta Percreta Involving the Urinary Bladder
- A case of placenta previa percreta with bladder invasion
- A Clinical Study of Placenta Previa
- A Case of Placenta Previa-Percreta Treated with Methotrexate Treatment