Korean J Ophthalmol.
2013 Dec;27(6):470-473. 10.3341/kjo.2013.27.6.470.
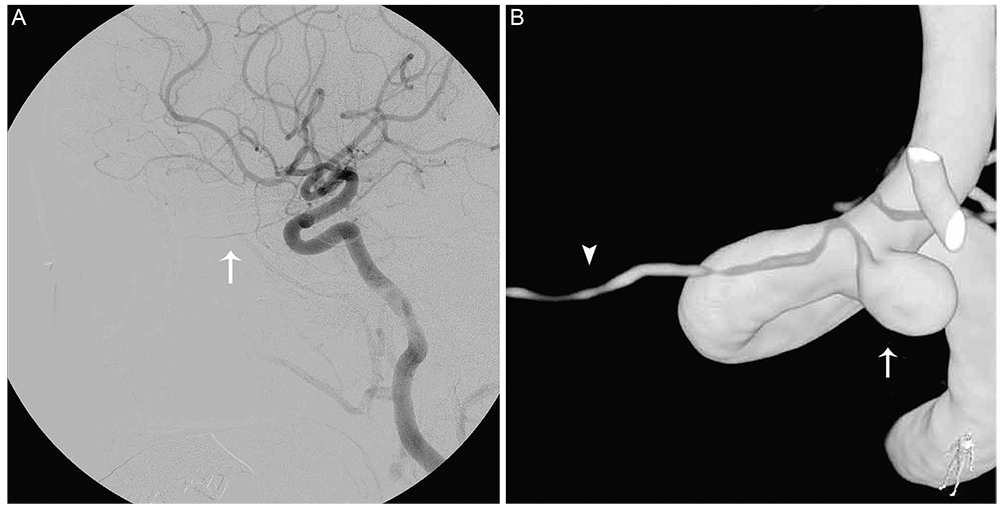
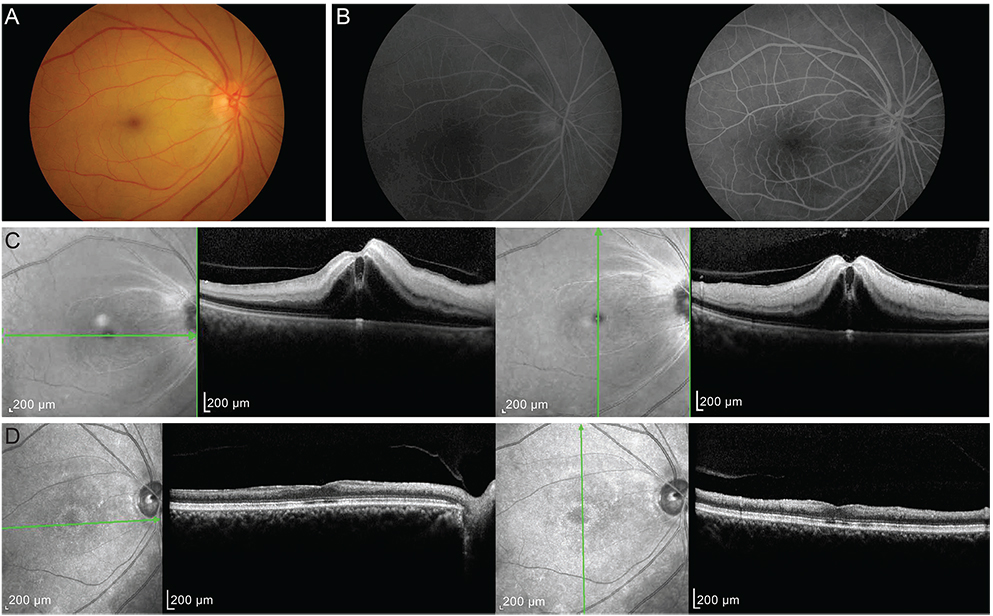
Ophthalmic Artery Aneurysm: Potential Culprit of Central Retinal Artery Occlusion
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Ophthalmology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. sejoon1@snu.ac.kr
- 3Department of Ophthalmology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Neurosurgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- KMID: 1792086
- DOI: http://doi.org/10.3341/kjo.2013.27.6.470
Abstract
- Central retinal artery occlusion (CRAO) is one of the most devastating ophthalmic emergencies, causing acute painless visual loss in the affected eye. We describe the first case of acute non-arteritic CRAO associated with peripheral ophthalmic artery aneurysm and its clinical course after intra-arterial thrombolysis therapy. This case suggests that ophthalmic artery aneurysm can be the cause of CRAO and should be included in the differential diagnosis of CRAO.
MeSH Terms
Figure
Reference
-
1. Rumelt S, Dorenboim Y, Rehany U. Aggressive systematic treatment for central retinal artery occlusion. Am J Ophthalmol. 1999; 128:733–738.2. Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion: associated systemic and ophthalmic abnormalities. Ophthalmology. 2009; 116:1928–1936.3. Qiao L, Wang H, Mao L, et al. Peripheral ophthalmic artery aneurysm. Neurosurg Rev. 2011; 34:29–38.4. Qureshi AI, Mohammad Y, Yahia AM, et al. Ischemic events associated with unruptured intracranial aneurysms: multicenter clinical study and review of the literature. Neurosurgery. 2000; 46:282–289.5. Haritoglou C, Muller-Schunk S, Weber C, et al. Central retinal artery occlusion in association with an aneurysm of the internal carotid artery. Am J Ophthalmol. 2001; 132:270–271.6. Bederson JB, Awad IA, Wiebers DO, et al. Recommendations for the management of patients with unruptured intracranial aneurysms: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Circulation. 2000; 102:2300–2308.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incomplete Central Retinal Artery Occlusion
- Intra-arterial Thrombolysis for Central Retinal Artery Occlusion after the Coil Embolization of Paraclinoid Aneurysm
- Central Retinal Artery Occlusion Masquerading as Branch Retinal Artery Occlusion
- Embolization through the Ophthalmic Artery with Onyx in Bilateral Ethmoidal Dural Arteriovenous Fistula: A Case Report
- The Successful Treatment of a Case of Central Retinal Artery Occlusion