Clin Orthop Surg.
2013 Dec;5(4):292-297. 10.4055/cios.2013.5.4.292.
The Effect of Zoledronic Acid on the Volume of the Fusion-Mass in Lumbar Spinal Fusion
- Affiliations
-
- 1Department of Orthopaedic Surgery, Guri Hospital, Hanyang University College of Medicine, Guri, Korea. hyparkys@hanyang.ac.kr
- 2Department of Radiology, Guri Hospital, Hanyang University College of Medicine, Guri, Korea.
- KMID: 1787032
- DOI: http://doi.org/10.4055/cios.2013.5.4.292
Abstract
- BACKGROUND
Few studies have explored the effects of bisphosphonates on bony healing in patients undergoing spinal fusion surgery. Most previous studies used animal models and found that bisphosphonate shows negative effects on spinal fusion consolidation. We intended to evaluate the effect of a single-dose of zoledronic acid on the volume of the fusion-mass in lumbar spinal fusion.
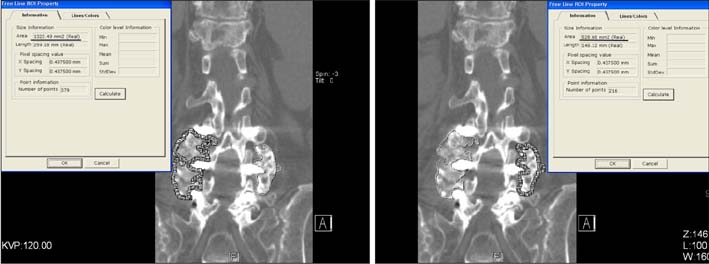
METHODS
A retrospective review was carried out on 44 patients with symptomatic degenerative lumbar spinal stenosis who underwent one or two-level posterolateral fusion from January 2008 and January 2011. They were divided into 4 groups: group 1, autograft and zoledronic acid; group 2, allograft and zoledronic acid; group 3, autograft alone; and group 4, allograft alone. Functional radiography and three-dimensional computed tomography scans were used to evaluate and quantify the volume of the fusion-mass. The visual analog scale (VAS), the Oswestry disability index (ODI), and the short form 36 (SF-36) were used to evaluate the clinical outcomes.
RESULTS
The mean volume of the fusion-mass per level was 8,814 mm3, 8,035 mm3, 8,383 mm3, and 7,550 mm3 in groups 1, 2, 3, and 4, respectively, but there were no significant differences between the groups (p = 0.829). There were no significant decreases in the volume of the fusion-mass (p = 0.533) in the zoledronic acid groups (groups 1 and 2). The VAS, the ODI, and the SF-36 at the 6-month follow-up after surgery were not significantly different (p > 0.05) among the 4 groups. The VAS, the ODI, and the SF-36 were not correlated with the volume of the fusion-mass (p = 0.120, 0.609, 0.642).
CONCLUSIONS
A single dose of zoledronic acid does not decrease the volume of the fusion-mass in patients undergoing spinal fusion with osteoporosis. Therefore, we recommend that zoledronic acid may be used after spinal fusion in osteoporotic patients.
MeSH Terms
-
Aged
Aged, 80 and over
Bone Density Conservation Agents/*therapeutic use
Diphosphonates/*therapeutic use
Female
Humans
Imidazoles/*therapeutic use
Lumbar Vertebrae/drug effects/pathology/radiography/surgery
Male
Middle Aged
Osteoporosis/drug therapy
Pain Measurement
Pain, Postoperative
Quality of Life
Retrospective Studies
Spinal Fusion/adverse effects/*methods
Spinal Stenosis/pathology/radiography/*surgery
Treatment Outcome
Bone Density Conservation Agents
Diphosphonates
Imidazoles
Figure
Reference
-
1. Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976). 2005; 30(12):1441–1445.
Article2. Katz JN. Lumbar spinal fusion: surgical rates, costs, and complications. Spine (Phila Pa 1976). 1995; 20:24 Suppl. 78S–83S.3. Greenspan SL, Maitland LA, Myers ER, Krasnow MB, Kido TH. Femoral bone loss progresses with age: a longitudinal study in women over age 65. J Bone Miner Res. 1994; 9(12):1959–1965.
Article4. Nagahama K, Kanayama M, Togawa D, Hashimoto T, Minami A. Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial. J Neurosurg Spine. 2011; 14(4):500–507.
Article5. Fisher JE, Rogers MJ, Halasy JM, et al. Alendronate mechanism of action: geranylgeraniol, an intermediate in the mevalonate pathway, prevents inhibition of osteoclast formation, bone resorption, and kinase activation in vitro. Proc Natl Acad Sci U S A. 1999; 96(1):133–138.
Article6. Hughes DE, Wright KR, Uy HL, et al. Bisphosphonates promote apoptosis in murine osteoclasts in vitro and in vivo. J Bone Miner Res. 1995; 10(10):1478–1487.
Article7. Huang RC, Khan SN, Sandhu HS, et al. Alendronate inhibits spine fusion in a rat model. Spine (Phila Pa 1976). 2005; 30(22):2516–2522.8. Babat LB, McLain R, Milks R, Ferrara L, Sohn MJ. The effects of the antiresorptive agents calcitonin and pamidronate on spine fusion in a rabbit model. Spine J. 2005; 5(5):542–547.9. Lehman RA Jr, Kuklo TR, Freedman BA, Cowart JR, Mense MG, Riew KD. The effect of alendronate sodium on spinal fusion: a rabbit model. Spine J. 2004; 4(1):36–43.10. Takahata M, Ito M, Abe Y, Abumi K, Minami A. The effect of anti-resorptive therapies on bone graft healing in an ovariectomized rat spinal arthrodesis model. Bone. 2008; 43(6):1057–1066.11. Little DG, Smith NC, Williams PR, et al. Zoledronic acid prevents osteopenia and increases bone strength in a rabbit model of distraction osteogenesis. J Bone Miner Res. 2003; 18(7):1300–1307.12. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992; 30(6):473–483.13. Bransford R, Goergens E, Briody J, Amanat N, Cree A, Little D. Effect of zoledronic acid in an L6-L7 rabbit spine fusion model. Eur Spine J. 2007; 16(4):557–562.14. Black DM, Delmas PD, Eastell R, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007; 356(18):1809–1822.15. Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007; 357(18):1799–1809.16. Colon-Emeric C, Nordsletten L, Olson S, et al. Association between timing of zoledronic acid infusion and hip fracture healing. Osteoporos Int. 2011; 22(8):2329–2336.17. Lin JT, Lane JM. Bisphosphonates. J Am Acad Orthop Surg. 2003; 11(1):1–4.18. Reid IR, Brown JP, Burckhardt P, et al. Intravenous zoledronic acid in postmenopausal women with low bone mineral density. N Engl J Med. 2002; 346(9):653–661.19. Moroni A, Faldini C, Hoang-Kim A, Pegreffi F, Giannini S. Alendronate improves screw fixation in osteoporotic bone. J Bone Joint Surg Am. 2007; 89(1):96–101.20. Xue Q, Li H, Zou X, et al. Alendronate treatment improves bone-pedicle screw interface fixation in posterior lateral spine fusion: an experimental study in a porcine model. Int Orthop. 2010; 34(3):447–451.21. Glassman SD, Dimar JR, Carreon LY, Campbell MJ, Puno RM, Johnson JR. Initial fusion rates with recombinant human bone morphogenetic protein-2/compression resistant matrix and a hydroxyapatite and tricalcium phosphate/collagen carrier in posterolateral spinal fusion. Spine (Phila Pa 1976). 2005; 30(15):1694–1698.22. Singh K, Smucker JD, Gill S, Boden SD. Use of recombinant human bone morphogenetic protein-2 as an adjunct in posterolateral lumbar spine fusion: a prospective CT-scan analysis at one and two years. J Spinal Disord Tech. 2006; 19(6):416–423.23. Seo WY, Park YS, Cho JL. Does a radiolucent zone surrounding the pedicle screws mean nonunion? J Korean Orthop Assoc. 2009; 44(3):344–349.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Severe Retrolisthesis at the Adjacent Segment after Lumbar Fusion Combined with Dynamic Stabilization
- Functional Recovery Program after Lumbar Spinal Fusion
- Volumetric Assessment of Fusion Mass and Its Clinical Correlations in Posterior Lumbar Interbody Fusion Depending on the Type of Bone Graft
- Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Arthroscopy
- Local Bone versus Autogenous Iliac Bone Graft for Posterolateral Lumbar Fusion in the Same Patient