J Korean Med Sci.
2011 Jun;26(6):803-806. 10.3346/jkms.2011.26.6.803.
Effects of Level of Consciousness on Urodynamic Procedure in Female Cats
- Affiliations
-
- 1Department of Urology and Andrology, Ninth People's Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai, China and Department of Urology, Seoul National University Hospital, Seoul, Korea.
- 2Laboratory of Veterinary Surgery, College of Veterinary Medicine, Chungbuk National University, Cheongju, Korea.
- 3Department of Urology, Seoul National University Hospital, Seoul and Neuroscience Research Institute, Medical Research Center, Seoul National University, Seoul, Korea. sjo@snu.ac.kr
- KMID: 1785968
- DOI: http://doi.org/10.3346/jkms.2011.26.6.803
Abstract
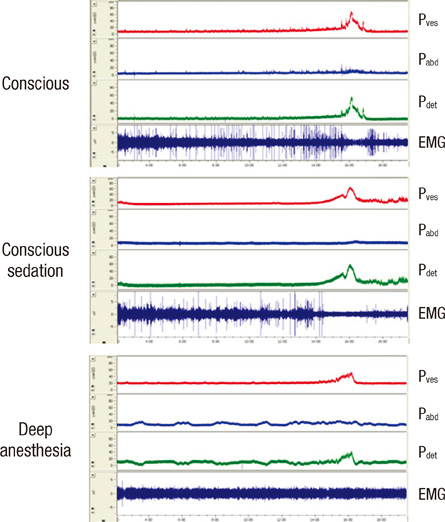
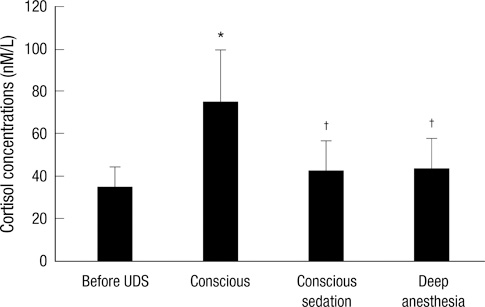
- Urodynamic evaluation is an invasive and uncomfortable procedure that can cause physical distress and is difficult to perform in uncooperative patients. The aim of this study was to evaluate the effects of consciousness on urodynamic evaluation in an animal model. Repeated cystometry, electromyogram, and measurement of serum cortisol concentrations were performed in female cats under conscious (CON), conscious sedation (CS) and deep anesthesia (DA) conditions. Urodynamic evaluation showed that there were no statistical differences in maximum detrusor pressure or bladder capacity observed among the three conditions. Under the DA condition, but not the CON and CS conditions, bladder contraction was accompanied by an un-relaxed anal sphincter. Residue urine volume significantly increased in the DA condition compared to the CON and CS conditions. The levels of serum cortisol significantly increased after performing urodynamic evaluation under the CON condition, whereas these levels were not significantly increased under the CS and DA conditions. This study showed that conscious sedation has no adverse effects on the urodynamic variables, and that it significantly reduces distress in cats undergoing the examination. These results may provide novel insights for performing urodynamic studies in uncooperative patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Blaivas J, Chancellor MB, Weiss J, Verhaaren M. Atlas of Urodynamics. 2007. 2nd ed. Blackwell;25.2. Park SH, Jin LH, Kwon YH, Yoon SM, Ryu JK, Lee T. Application and limitations of awake cystometry in Sprague-Dawley rats with partial bladder outlet obstruction as a model of overactive bladder or obstruction. Korean J Urol. 2009. 50:486–492.3. Cohen TA, Westropp JL, Kass PH, Pypendop BH. Evaluation of urodynamic procedures in female cats anesthetized with low and high doses of isoflurane and propofol. Am J Vet Res. 2009. 70:290–296.4. Chang HY, Havton LA. Differential effects of urethane and isoflurane on external urethral sphincter electromyography and cystometry in rats. Am J Physiol Renal Physiol. 2008. 295:F1248–F1253.5. Cannon TW, Damaser MS. Effects of anesthesia on cystometry and leak point pressure of the female rat. Life Sci. 2001. 69:1193–1202.6. Ghoniem GM, Shoukry MS, Monga M. Effects of anesthesia on urodynamic studies in the primate model. J Urol. 1996. 156:233–236.7. Merguerian PA, Corbett ST, Cravero J. Voiding ability using propofol sedation in children undergoing voiding cystourethrograms: a retrospective analysis. J Urol. 2006. 176:299–302.8. Tosun Z, Aksu R, Guler G, Esmaoglu A, Akin A, Aslan D, Boyaci A. Propofol-ketamine vs propofol-fentanyl for sedation during pediatric upper gastrointestinal endoscopy. Paediatr Anaesth. 2007. 17:983–988.9. Lee JS, Gonzalez ML, Chuang SK, Perrott DH. Comparison of methohexital and propofol use in ambulatory procedures in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2008. 66:1996–2003.10. Ku JH, Kim SW, Kim HH, Paick JS, Son H, Oh SJ. Patient experience with a urodynamic study: a prospective study in 208 patients. J Urol. 2004. 171:2307–2310.11. Doshani A, Mayne C, Tincello D. Anxiety among women attending urodynamic investigation: scoping study for a randomized trial of psychometric intervention. Neurourol Urodyn. 2009. 28:177–178.12. Willemse T, Vroom MW, Mol JA, Rijnberk A. Changes in plasma cortisol, corticotropin, and alpha-melanocyte-stimulating hormone concentrations in cats before and after physical restraint and intradermal testing. Am J Vet Res. 1993. 54:69–72.13. Yoder B, Wolf JS Jr. Canine model of surgical stress response comparing standard laparoscopic, microlaparoscopic, and hand-assisted laparoscopic nephrectomy. Urology. 2005. 65:600–603.14. Committee on Drugs. American Academy of Pediatrics. Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: addendum. Pediatrics. 2002. 110:836–838.15. Lee CC, Lin YY, Hsu CW, Chu SJ, Tsai SH. Movement disorder caused by abuse of veterinary anesthesia containing tiletamine. Am J Emerg Med. 2009. 27:1022e5–e6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship between the Level of I-conscousness We-consciousness and Interpersonal Problems of Korean Medical Students
- Two Cases of Urodynamic Improvements after Mesh Resection in Patients with Protracted Urinary Retention Following Tension-free Vaginal Tape
- Experimental Cerebral Infarction Following Occlusion of Middle Cerebral Artery
- The factors of pain and anxiety associated with urodynamics in female patients
- The Effect of Naloxone on Pathological Changes in the Experimental Spinal Cord Injury