J Korean Acad Nurs.
2012 Jun;42(3):424-433. 10.4040/jkan.2012.42.3.424.
Accuracy, Precision, and Validity of Fever Detection using Non-invasive Temperature Measurement in Adult Coronary Care Unit Patients with Pulmonary Catheters
- Affiliations
-
- 1Department of Nursing, Kyungin Women's College, Incheon, Korea.
- 2College of Nursing, The Catholic University of Korea, Seoul, Korea. sky@catholic.ac.kr
- KMID: 1785227
- DOI: http://doi.org/10.4040/jkan.2012.42.3.424
Abstract
- PURPOSE
To investigate the accuracy, precision and validity of fever detection of tympanic membrane (TM), temporal artery (TA) and axillary temperature (AT) compared with pulmonary artery temperature (PA).
METHODS
Repeated-measures design was conducted for one year on 83 adult cardiac care unit patients with pulmonary artery catheters after open heart surgery. Sequential temperature measurements were taken three times at 20-minute intervals. Accuracy, precision, repeatability, and validity of fever detection were analyzed.
RESULTS
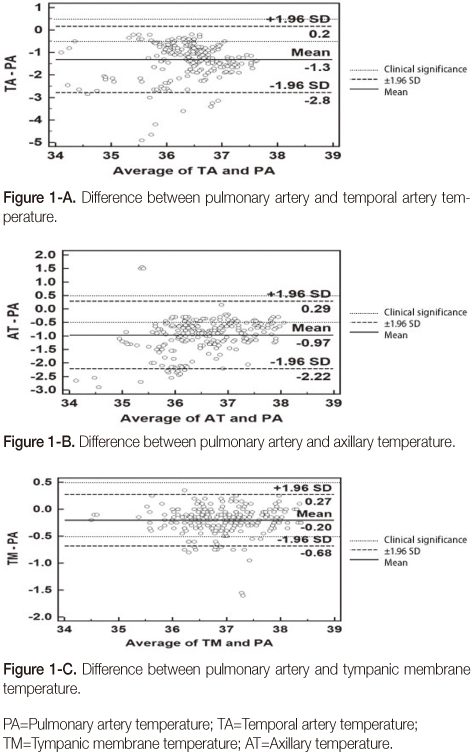
Mean pulmonary artery temperature was 37.04degrees C (SD 0.70degrees C). The mean (SD) offsets from PA, with the mean reflecting accuracy and SD reflecting precision, were -1.31degrees C (0.75degrees C) for TA, -0.20degrees C (0.24degrees C) for TM, and -0.97degrees C (0.64degrees C) for AT. Percentage of pairs with differences within +/-0.5degrees C was 9.6% for TA, 19.7% for AT, and 91.6% for TM. Repeated measurements with all three methods had mean SD values within 0.04degrees C. Sensitivity, specificity, and positive and negative predictive values of tympanic measurements were 0.76, 1.0, and 1.0, and 0.90, respectively.
CONCLUSION
Results show that TM best reflects PA, and is most consistent, accurate, and precise. AT tends to underestimate PA, and TA is least accurate and precise. Therefore tympanic membrane measurement is a reliable alternative to other non-invasive methods of measuring temperatures.
Keyword
MeSH Terms
Figure
Reference
-
1. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986. 1:307–310.2. Brooks S, Khan A, Stoica D, Griffith J, Friedeman L, Mukherji R, et al. Reduction in vancomycin-resistant Enterococcus and Clostridium difficile infections following change to tympanic thermometers. Infection Control and Hospital Epidemiology. 1998. 19:333–336. http://dx.doi.org/10.1086/647824.3. Carroll D, Finn C, Judge B, Gill S, Sawyer J. A comparison of measurements from a temporal artery thermometer and a pulmonary artery catheter thermistor. American Journal of Critical Care. 2004. 13:258.4. Cattaneo CG, Frank SM, Hesel TW, El-Rahmany HK, Kim LJ, Tran KM. The accuracy and precision of body temperature monitoring methods during regional and general anesthesia. Anesthesia and Analgesia. 2000. 90:938–945. http://dx.doi.org/10.1097/00000539-200004000-00030.5. Craig JV, Lancaster GA, Taylor S, Williamson PR, Smyth RL. Infrared ear thermometry compared with rectal thermometry in children: A systematic review. Lancet. 2002. 360:603–609. http://dx.doi.org/10.1016/S0140-6736(02)09783-0.6. Giuliano KK, Giuliano AJ, Scott SS, MacLachlan E, Pysznik E, Elliot S, et al. Temperature measurement in critically ill adults: A comparison of tympanic and oral methods. American Journal of Critical Care. 2000. 9:254–261.7. Greenes DS, Fleisher GR. Accuracy of a noninvasive temporal artery thermometer for use in infants. Archives of Pediatrics and Adolescent Medicine. 2001. 155:376–381.8. Hwang JS, Sohng KY. Comparison of rectal temperature with axillary and tympanic temperature. Journal of Korean Academy of Fundamentals of Nursing. 1997. 4:351–358.9. Kenney RD, Fortenberry JD, Surratt SS, Ribbeck BM, Thomas WJ. Evaluation of an infrared tympanic membrane thermometer in pediatric patients. Pediatrics. 1990. 85:854–858.10. Kimberger O, Cohen D, Illievich U, Lenhardt R. Temporal artery versus bladder thermometry during perioperative and intensive care unit monitoring. Anesthesia and Analgesia. 2007. 105:1042–1047. http://dx.doi.org/10.1213/01.ane.0000281927.88935.e0.11. Kistemaker JA, DenHartog EA, Daanen HA. Reliability of an infrared forehead skin thermometer for core temperature measurements. Journal of Medical Engineering and Technology. 2006. 30:252–261. http://dx.doi.org/10.1080/03091900600711381.12. Koo HY, Son JT. Comparison of inguinal, rectal, axillary, and tympanic temperature in newborns. Korean Journal of Child Health Nursing. 2005. 11:203–210.13. Koo SH, Jeong MS, Kim KA, Ko SY, Lee YK, Shin SM. Comparison of body temperature measured by non-contact temporal artery thermometer with those by other methods in neonates. Korean Journal of Perinatology. 2003. 14:409–415.14. Korean Society for the Study of Obesity. The Asia-Pacific perspective: Redefining obesity and its treatment. 2006. 02. Seoul: Author;(Original work published 2000).15. Lawson L, Bridges EJ, Ballou I, Eraker R, Greco S, Shively J, et al. Accuracy and precision of noninvasive temperature measurement in adult intensive care patients. American Journal of Critical Care. 2007. 16:485–496.16. Lee WH, Jung SP. The validity of the tympanic membrane thermometer in detecting fever of the children. Journal of the Korean Academy of Family Medicine. 1995. 16:531–536.17. Marable K, Shaffer LE, Dizon V, Opalek JM. Temporal artery scanning falls short as a secondary, noninvasive thermometry method for trauma patients. Journal of Trauma Nursing. 2009. 16:41–47. http://dx.doi.org/10.1097/01.JTN.0000348069.71593.9d.18. Myny D, De Waele J, Defloor T, Blot S, Colardyn F. Temporal scanner thermometry: A new method of core temperature estimation in ICU patients. Scottish Medical Journal. 2005. 50:15–18.19. Park CW, Park SN. Development of standard and improvement of reliability in body temperature measurement. Journal of the Korean Society of Precision Engineering. 2007. 24(9):32–36.20. Potter PA, Perry AG, Stockert P. Basic nursing. 2010. St. Louis: Mosby Co.21. Ronneberg K, Roberts WO, McBean AD, Center BA. Temporal artery temperature measurements do not detect hyperthermic marathon runners. Medicine and Science in Sports and Exercise. 2008. 40:1373–1375. http://dx.doi.org/10.1249/MSS.0b013e31816d65bb.22. Shiraki K, Konda N, Sagawa S. Esophageal and tympanic temperature responses to core blood temperature changes during hyperthermia. Journal of Applied Physiology. 1986. 61:98–102.23. Siberry GK, Diener-West M, Schappell E, Karron RA. Comparison of temple temperatures with rectal temperature in children under two years of age. Clinical Pediatrics. 2002. 41:405–414. http://dx.doi.org/10.1177/000992280204100605.24. Sohng KY, Park HS, Hong YH, Yun EJ, Lee KY, Cho BH. Fundamentals of nursing. 2009. Seoul: Soomoonsa.25. Suleman MI, Doufas AG, Akça O, Ducharme M, Sessler DI. Insufficiency in a new temporal-artery thermometer for adult and pediatric patients. Anesthesia and Analgesia. 2002. 95:67–71. http://dx.doi.org/10.1097/00000539-200207000-00012.26. Yoo JH, Jo HS. Comparison of tympanic and axillary temperatures. Journal of Korean Academy of Fundamentals of Nursing. 2009. 16:162–170.27. Yun KW, Lim IS. A study for accuracy and usefulness of tympanic membrane and forehead thermometers. Korean Journal of Pediatrics. 2005. 48:820–825.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy of Temperature Measurements, Nursing Time for Measuring Temperature and the Validity of Fever Detection
- Diagnostic Accuracy of Temporal Artery Temperatures Measurements
- Appropriate Body Temperature Measurement Method for Parents of Infants
- Reliability and Accuracy of Infrared Temperature: A Systematic Review
- Comparison of Rectal Temperature with Axillary and Tympanic Temperature