Clin Orthop Surg.
2014 Jun;6(2):223-229. 10.4055/cios.2014.6.2.223.
What Is the Usefulness of the Fragmentation Pattern of the Femoral Head in Managing Legg-Calve-Perthes Disease?
- Affiliations
-
- 1Department of Orthopaedic Surgery, Pusan National University Hospital, Busan, Korea. kimht@pusan.ac.kr
- 2Department of Rheumatology, Pusan National University Hospital, Busan, Korea.
- 3Center for Excellence in Hip Disorders, Texas Scottish Rite Hospital for Children, Dallas, TX, USA.
- 4Department of Orthopaedic Surgery, University of Texas Southwestern Medical Center, Dallas, TX, USA.
- KMID: 1784671
- DOI: http://doi.org/10.4055/cios.2014.6.2.223
Abstract
- BACKGROUND
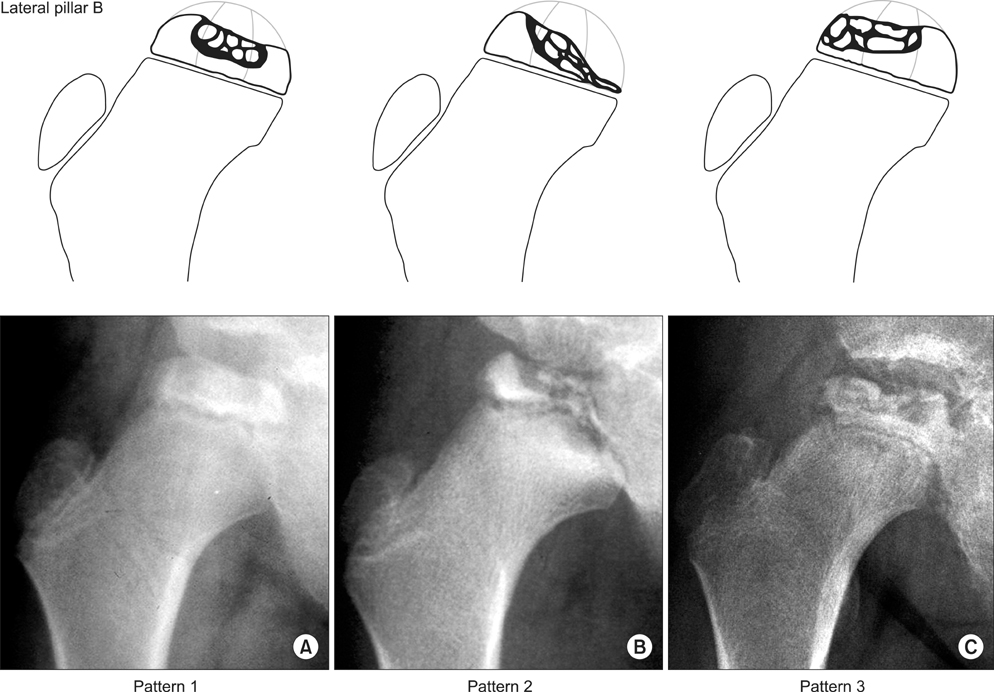
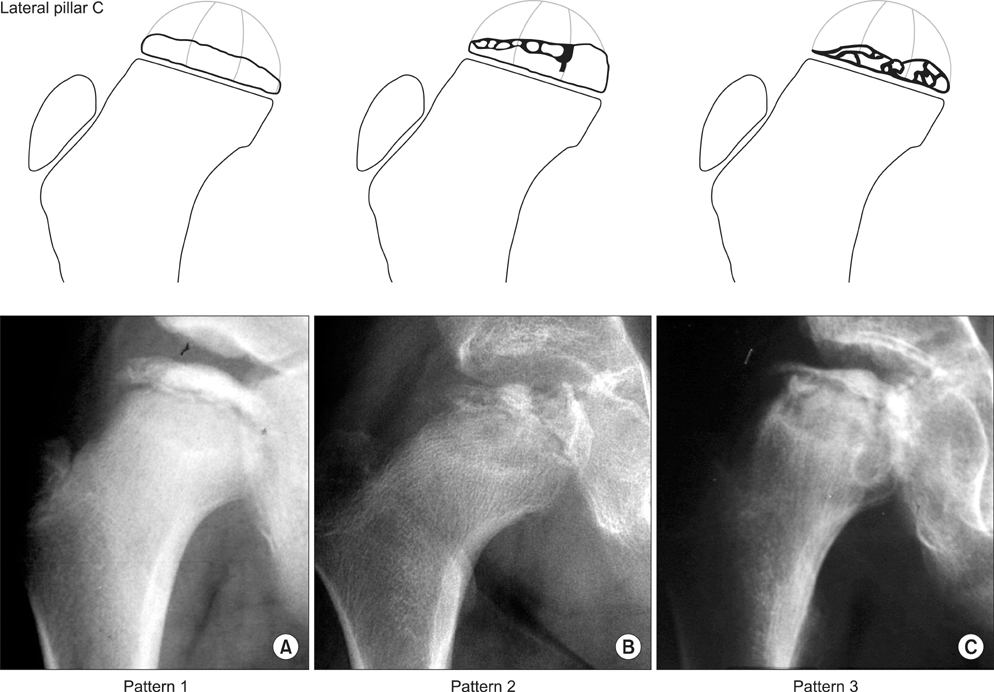
Within the lateral pillar classification of the Legg-Calve-Perthes (LCP) disease, hips seem quite variable in the pattern of fragmentation as seen in radiographs. The purpose of this study was to determine: if it is possible to reliably subdivide the lateral pillar groups into femoral head fragmentation patterns, and if such a subdivision of the lateral pillar groupings is clinically useful in managing LCP disease.
METHODS
Two hundred and ninety-three anteroposterior radiographs taken at the maximal fragmentation stage (189 lateral pillar B, 57 B/C border, and 47 C hips; mean bone/chronologic age at the time of first visit, 6.2/7.9 years) and at skeletal maturity (mean age, 16.6 years) were analyzed. We distinguished 3 fragmentation patterns in each pillar group based on the region of major involvement. We tested the inter- and intraobserver reliability of our classification system and analyzed the relationships between the fragmentation patterns and the Stulberg outcomes as well as other factors such as surgical treatment and age.
RESULTS
Inter- and intraobserver consistency in fragmentation pattern assignments was found to be substantial to excellent. A statistically significant trend (p = 0.001) in the proportion of Stulberg III or IV outcomes in comparison with Stulberg I and II was only found for the different fragmentation patterns in our lateral pillar B patients: fragmentation patterns having mainly lateral-central necrosis led to poor outcomes. No significant association was found between fragmentation patterns and Stulberg outcomes in pillar groups B/C border and C.
CONCLUSIONS
Our results are consistent with the lateral pillar classification itself. Therefore, fragmentation patterns in each lateral pillar classification did not provide clinical usefulness in the management of LCP disease.
MeSH Terms
Figure
Reference
-
1. Catterall A. The natural history of Perthes' disease. J Bone Joint Surg Br. 1971; 53(1):37–53.2. Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part I: classification of radiographs with use of the modified lateral pillar and Stulberg classifications. J Bone Joint Surg Am. 2004; 86(10):2103–2120.3. Herring JA, Neustadt JB, Williams JJ, Early JS, Browne RH. The lateral pillar classification of Legg-Calvé-Perthes disease. J Pediatr Orthop. 1992; 12(2):143–150.4. Kuroda T, Mitani S, Sugimoto Y, et al. Changes in the lateral pillar classification in Perthes' disease. J Pediatr Orthop B. 2009; 18(3):116–119.5. Lappin K, Kealey D, Cosgrove A. Herring classification: how useful is the initial radiograph? J Pediatr Orthop. 2002; 22(4):479–482.6. Park MS, Chung CY, Lee KM, Kim TW, Sung KH. Reliability and stability of three common classifications for Legg-Calvé-Perthes disease. Clin Orthop Relat Res. 2012; 470(9):2376–2382.7. Nathan Sambandam S, Gul A, Shankar R, Goni V. Reliability of radiological classifications used in Legg-Calve-Perthes disease. J Pediatr Orthop B. 2006; 15(4):267–270.8. Podeszwa DA, Stanitski CL, Stanitski DF, Woo R, Mendelow MJ. The effect of pediatric orthopaedic experience on interobserver and intraobserver reliability of the herring lateral pillar classification of Perthes disease. J Pediatr Orthop. 2000; 20(5):562–565.9. Ritterbusch JF, Shantharam SS, Gelinas C. Comparison of lateral pillar classification and Catterall classification of Legg-Calvé-Perthes' disease. J Pediatr Orthop. 1993; 13(2):200–202.10. Simmons ED, Graham HK, Szalai JP. Interobserver variability in grading Perthes' disease. J Bone Joint Surg Br. 1990; 72(2):202–204.11. Greulich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. 2nd ed. Stanford, CA: Stanford University Press;1959.12. Acheson RM. The Oxford method of assessing skeletal maturity. Clin Orthop. 1957; 10:19–39.13. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33(1):159–174.14. Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part II: prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004; 86(10):2121–2134.15. Bland JM, Altman DG. Statistics notes: the odds ratio. BMJ. 2000; 320(7247):1468.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osteochondritis Dissecans of Femoral Head Following Legg-Calve-Perthes Disease
- Clinical Observation of the Legg-Calve-Perthes Disease: Preliminary Report
- Partial Capital Resection in Legg-Calve-Perthes' Diseases
- Innominate Osteotomy in Legg-Calve-Perthes Disease
- Legg - Calve Perthes disease in Monozygotic Male Twins