Neurointervention.
2012 Feb;7(1):40-44. 10.5469/neuroint.2012.7.1.40.
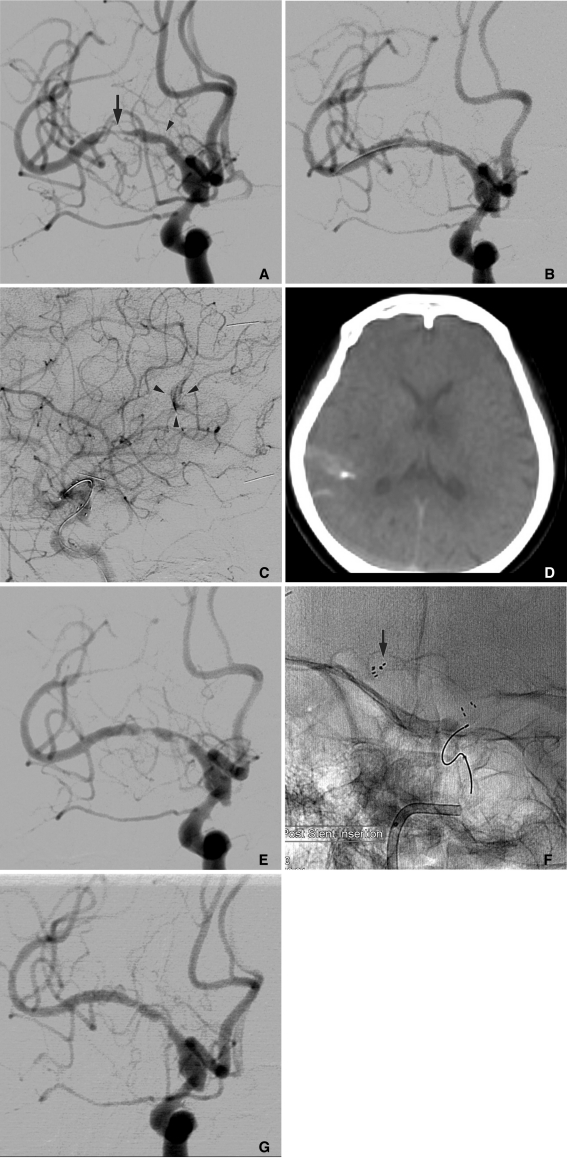
Coincidental Occurrence of Acute In-stent Thrombosis and Iatrogenic Vessel Perforation During a Wingspan Stent Placement: Management with a Stent In-stent Technique
- Affiliations
-
- 1Department of Neurosurgery, Kyung Hee University Hospital at Gangdong, Seoul, Korea. gjs@khnmc.or.kr
- KMID: 1783998
- DOI: http://doi.org/10.5469/neuroint.2012.7.1.40
Abstract
- We presented a case that an acute in-stent thrombosis after the deployment of a Wingspan stent was successfully managed with a stent in-stent technique. Because vessel perforation and subarachnoid hemorrhage were iatrogenically developed during the procedure, we were unable to use the thrombolytic agents to correct the in-stent thrombosis. When a thrombotic complication following an intracranial stent placement occurs with a coincidentally hemorrhagic complication, the stent in-stent technique should be considered as a treatment option.
MeSH Terms
Figure
Reference
-
1. Chimowitz MI, Kokkinos J, Strong J, Brown MB, Levine SR, Silliman S, et al. The warfarin-aspirin symptomatic intracranial disease study. Neurology. 1995; 45:1488–1493. PMID: 7644046.
Article2. Bose A, Hartmann M, Henkes H, Liu HM, Teng MM, Szikora I, et al. A novel, self-expanding, nitinol stent in medically refractory intracranial atherosclerotic stenoses: the Wingspan study. Stroke. 2007; 38:1531–1537. PMID: 17395864.3. Fiorella D, Levy EI, Turk AS, Albuquerque FC, Niemann DB, Aagaard-Kienitz B, et al. US multicenter experience with the Wingspan stent system for the treatment of intracranial atheromatous disease: periprocedural results. Stroke. 2007; 38:881–887. PMID: 17290030.
Article4. Lawson MF, Fautheree GL, Waters MF, Decker DA, Mocco JD, Hoh BL. Acute intraprocedural thrombus formation during Wingspan intracranial stent placement for intracranial atherosclerotic disease. Neurosurgery. 2010; 67:ons166–ons170. PMID: 20679932.
Article5. Fiorella DJ, Levy EI, Turk AS, Albuquerque FC, Pride GL Jr, Woo HH, et al. Target lesion revascularization after Wingspan: assessment of safety and durability. Stroke. 2009; 40:106–110. PMID: 18927447.6. Riedel CH, Tietke M, Alfke K, Stingele R, Jansen O. Subacute stent thrombosis in intracranial stenting. Stroke. 2009; 40:1310–1314. PMID: 19213948.
Article7. Grossmann R, Sokolova O, Schnurr A, Bonz A, Porsche C, Obergfell A, et al. Variable extent of clopidogrel responsiveness in patients after coronary stenting. Thromb Haemost. 2004; 92:1201–1206. PMID: 15583724.
Article8. Levy EI, Turk AS, Albuquerque FC, Niemann DB, Aagaard-Kienitz B, Pride L, et al. Wingspan in-stent restenosis and thrombosis: incidence, clinical presentation, and management. Neurosurgery. 2007; 61:644–650. PMID: 17881980.9. Le TM, Gaughen JR, Jensen ME, Evans AJ. Symptomatic Wingspan stent stenosis and occlusion: stent-in-stent rescue. J Neurointerv Surg. 2010; 2:348–350. PMID: 21990644.
Article10. Halbach VV, Higashida RT, Dowd CF, Barnwell SL, Hieshima GB. Management of vascular perforations that occur during neurointerventional procedures. AJNR Am J Neuroradiol. 1991; 12:319–327. PMID: 1902036.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Wingspan Stenting for Symptomatic Severe In-Stent Stenosis of a Closed-Cell Stent after Stent-Assisted Coiling of a Ruptured Intracranial Aneurysm
- Late Stent Thrombosis Associated with Late Stent Malapposition after Drug-Eluting Stenting: A Case Report
- Very Late Stent Thrombosis Related to Fracture of a Sirolimus-Eluting Stent
- Biliary Stent Placement for the Management of Acute Obstructive Jaundice after Uncovered Gastroduodenal Stent Placement
- Very Late Stent Thrombosis after Sole Stent-Assisted Coiling at the Paraclinoid Giant Aneurysm : Could Prophylactic Antiplatelet Therapy Be Ceased at the Only 1 Year after Procedure?