Infect Chemother.
2008 Jun;40(3):184-190. 10.3947/ic.2008.40.3.184.
A Case of 'True' Fungus-Infected Aneurysm of Abdominal Aorta in an Immunocompetent Patient
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, Soon Chun Hyang University, Seoul, Korea. geuncom@hosp.sch.ac.kr
- 2Department of Thoracic and Cardiovascular Surgery, College of Medicine, Soon Chun Hyang University, Seoul, Korea.
- 3Department of Radiology, College of Medicine, Soon Chun Hyang University, Seoul, Korea.
- 4Department of Pathology, College of Medicine, Soon Chun Hyang University, Seoul, Korea.
- KMID: 1782294
- DOI: http://doi.org/10.3947/ic.2008.40.3.184
Abstract
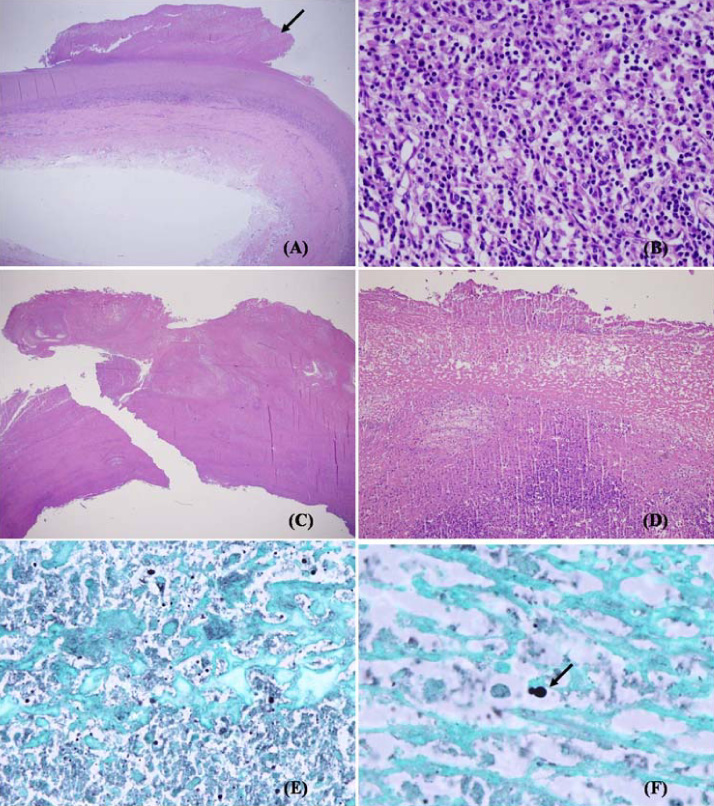
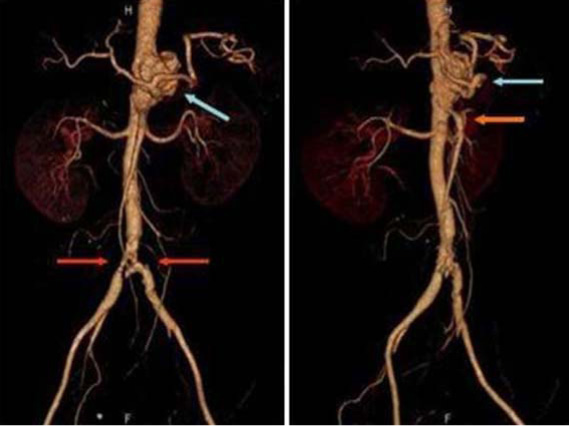
- Infected aneurysms are uncommon, frequently fatal lesions. "True" fungus-infected aneurysms are even rarer. Fungal infections have high morbidity and mortality. However, diagnosis is frequently difficult, since the symptoms are non-specific and standard diagnostic procedures are often insensitive. We experienced a patient with persistent fever and negative blood cultures. The patient was immunocompetent and had no risk factors, and was diagnosed with a fungus-infected aneurysm based on computed tomography and vascular surgery. The vascular tissue revealed some narrow-based budding yeast within the thrombus, suggesting Candida infection. Seventeen cases of infected aneurysm of the abdomen were reported in Korea from 1988 to 2007, although none were "true" fungus-infected aneurysms, making this the first fungus-infected aneurysm of the abdomen in Korea. Prompt diagnostic procedures and aggressive treatment modalities are necessary for patients with occult infection and negative blood cultures, regardless of their immunocompetence, because of the high morbidity and mortality of this condition.
Keyword
MeSH Terms
Figure
Reference
-
1. Parkhurst GF, Dekcer JP. Bacterial aortitis and mycotic aneurysm of the aorta; a report of twelve cases. Am J Pathol. 1955. 31:821–835.2. Oderich GS, Panneton JM, Bower TC, Cherry KJ, Rowland CM, Noel AA, Hallett JW, Gloviczki P. Infected aortic aneurysms: Aggressive presentation, complicated early outcome, but durable results. J Vasc Surg. 2001. 34:900–908.
Article3. Ewart JM, Burke ML, Bunt TJ. Spontaneous abdominal aortic infections. Essentials of diagnosis and management. Am Surg. 1983. 49:37–50.4. Potti A, Danielson B, Sen K. "True" mycotic aneurysm of a renal artery allograft. Am J Kidney Dis. 1998. 31:E3.
Article5. Werner K, Tarasoutchi F, Lunardi W, Mariño JC, Grinberg M, Bellotti G, Jatene AD. Mycotic aneurysm of the celiac trunk and superior mesenteric artery in a case of infective endocarditis. J Cardiovasc Surg (Torino). 1991. 32:380–383.6. Gauto AR, Cone LA, Woodard DR, Mahler RJ, Lynch RD, Stoltzman DH. Arterial infections due to Listeria monocytogenes: report of four cases and review of world literature. Clin Infect Dis. 1992. 14:23–28.
Article7. Walsh TJ, Hutchins GM. Aspergillus mural endocarditis. Am J Clin Pathol. 1979. 71:640–644.
Article8. Manuel RJ, Kibbler CC. The epidemiology and prevention of invasive aspergillosis. J Hosp Infect. 1998. 39:95–109.
Article9. Sanchez-Recalde A, Maté I, Merino JL, Simon RS, Sobrino JA. Aspergillus aortitis after cardiac surgery. J Am Coll Cardiol. 2003. 41:152–156.10. Fisher JF, Chew WH, Shadomy S, Duma RJ, Mayhall CG, House WC. Urinary tract infections due to Candida albicans. Rev Infect Dis. 1982. 4:1107–1118.
Article11. Davutoglu V, Soydinc S, Aydin A, Karakok M. Rapidly advancing invasive endomyocardial aspergillosis. J Am Soc Echocardiogr. 2005. 18:185–187.
Article12. Gonda RL Jr, Gutierrez OH, Azodo MV. Mycotic aneurysms of the aorta: radiologic features. Radiology. 1988. 168:343–346.
Article13. Ljungman P, von Döbeln L, Ringholm L, Lewensohn-Fuchs I, Klingspor L, Sparrelid E. The value of CMV and fungal PCR for monitoring for acute leukaemia and autologous stem cell transplant patients. Scand J Infect Dis. 2005. 37:121–127.14. Chung JW, Park SJ, Sung H, Kim MN, Kim BS, Lee SG. A Case of Disseminated Infection Due to Scedosporium apiospermum in a Liver-transplantation Recipient. Korean J Lab Med. 2005. 25:421–424.15. Rutherford RB. Vascular surgery. 1989. 3rd ed. Philadelphia: WB Saunders;969.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravascular Epithelioid Angiosarcoma in the Abdominal Aorta Mimicking an Infected Aneurysm
- Mycotic Aneurysm of Abdominal Aorta Causing the Right Renal Arterial Stenosis: Case Report
- Mycotic aneurysm of the abdominal aorta: a case report-
- A case of ruptured infected aneurysm of abdominal aorta caused by septic salmonellosis
- A Ruptured Salmonella-Infected Abdominal Aortic Aneurysm of the Suprarenal Type: A case report