J Korean Med Sci.
2012 Sep;27(9):1085-1090. 10.3346/jkms.2012.27.9.1085.
Antihypertensive Treatment of Acute Intracerebral Hemorrhage by Intravenous Nicardipine Hydrochloride: Prospective Multi-Center Study
- Affiliations
-
- 1Department of Neurosurgery, Ewha Womans University College of Medicine, Seoul, Korea. nshsg@ewha.ac.kr
- 2Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Neurosurgery, Seoul Medical Center, Seoul, Korea.
- 4Department of Neurosurgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Neurosurgery, National Health Insurance Corporation Ilsan Hospital, Goyang, Korea.
- KMID: 1782144
- DOI: http://doi.org/10.3346/jkms.2012.27.9.1085
Abstract
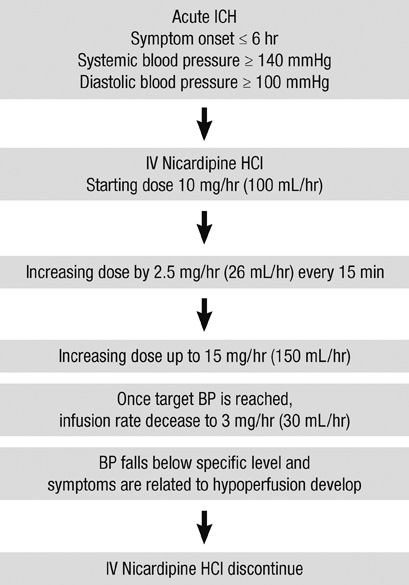
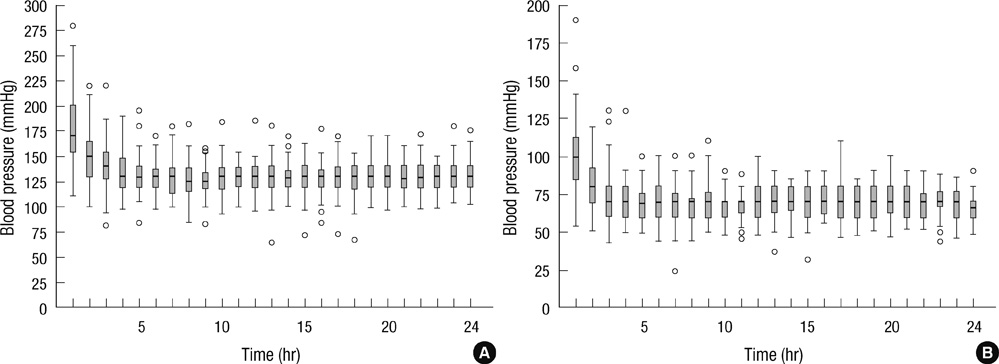
- The authors performed a multicenter prospective study to evaluate the feasibility and safety of intravenous nicardipine hydrochloride for acute hypertension in patients with intracerebral hemorrhage (ICH). This study included 88 patients (mean age: 58.3 yr, range 26-87 yr) with ICH and acute hypertension in 5 medical centers between August 2008 and November 2010, who were treated using intravenous nicardipine. Administration of nicardipine resulted in a decrease from mean systolic blood pressure (BP) (175.4 +/- 33.7 mmHg) and diastolic BP (100.8 +/- 22 mmHg) at admission to mean systolic BP (127.4 +/- 16.7 mmHg) and diastolic BP (67.2 +/- 12.9 mmHg) in 6 hr after infusion (P < 0.001, mixed-effect linear models). Among patients who underwent follow-up by computed tomography, hematoma expansion at 24 hr (more than 33% increase in hematoma size at 24 hr) was observed in 3 (3.4%) of 88 patients. Neurological deterioration (defined as a decrease in initial Glasgow coma scale > or = 2) was observed in 2 (2.2%) of 88 patients during the treatment. Aggressive nicardipine treatment of acute hypertension in patients with ICH can be safe and effective with a low rate of neurological deterioration and hematoma expansion.
MeSH Terms
-
Acute Disease
Adult
Aged
Aged, 80 and over
Antihypertensive Agents/adverse effects/*therapeutic use
Blood Pressure
Cerebral Hemorrhage/*drug therapy
Cohort Studies
Female
Follow-Up Studies
Glasgow Coma Scale
Hematoma/etiology
Humans
Injections, Intravenous
Male
Middle Aged
Nicardipine/adverse effects/*therapeutic use
Prospective Studies
Tomography, X-Ray Computed
Treatment Outcome
Antihypertensive Agents
Nicardipine
Figure
Cited by 2 articles
-
Comparative Analysis of the Patients with Spontaneous Thalamic Hemorrhage with Concurrent Intraventricular Hemorrhage and Those without Intraventricular Hemorrhage
Taek Min Nam, Ji Hwan Jang, Seung Hwan Kim, Kyu Hong Kim, Young Zoon Kim
J Korean Med Sci. 2020;36(1):e4. doi: 10.3346/jkms.2021.36.e4.Transcranial Doppler study in acute spontaneous intracerebral hemorrhage: The role of pulsatility index
Jiyong Park, Sung-Kyun Hwang
J Cerebrovasc Endovasc Neurosurg. 2021;23(4):334-342. doi: 10.7461/jcen.2021.E2021.05.001.
Reference
-
1. Anderson CS, Jamrozik KD, Broadhurst RJ, Stewart-Wynne EG. Predicting survival for 1 year among different subtypes of stroke: result from the Perth Community Stroke Group. Stroke. 1994. 25:1935–1944.2. Rasool AH, Rahman AR, Choudhury SR, Singh RB. Blood pressure in acute intracerebral haemorrhage. J Hum Hypertens. 2004. 18:187–192.3. Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF. Spontaneous intracerebral hemorrhage. N Engl J Med. 2001. 344:1450–1460.4. Broderick J, Brott T, Tomsick T, Tew J, Dulder J, Huster G. Management of intracerebral hemorrhage in a large metropolitan population. Neurosurgery. 1994. 34:882–887.5. Lisk DR, Pasteur W, Rhoades H, Putnam RD, Grotta JC. Early presentation of hemispheric intracerebral hemorrhage: prediction of outcome and guidelines for treatment allocation. Neurology. 1994. 44:133–139.6. Tuhrim S, Horowitz DR, Sacher M, Godbold JH. Validation and comparison of models predicting survival following intracerebral hemorrhage. Crit Care Med. 1995. 23:950–954.7. Juvela S. Risk factors for impaired outcome after spontaneous intracerebral hemorrhage. Arch Neurol. 1995. 52:1193–1200.8. Bullock R, Brock-Utne J, van Dellen J, Blake G. Intracerebral hemorrhage in a primate model: effect on regional cerebral blood flow. Surg Neurol. 1988. 29:101–107.9. Ohwaki K, Yano E, Nagashima H, Hirata M, Nakagomi T, Tamura A. Blood pressure management in acute intracerebral hemorrhage relationship between elevated blood pressure and hematoma enlargement. Stroke. 2004. 35:1364–1367.10. Qureshi AI, Mohammad YM, Yahia AM, Suarez JI, Siddiqui AM, Kirmani JF, Suri MF, Kolb J, Zaidat OO. A prospective multicenter study to evaluate the feasibility and safety of aggressive antihypertensive treatment in patients with acute intracerebral hermorrhage. J Intensive Care Med. 2005. 20:34–42.11. Maruishi M, Shima T, Okada Y, Nishida M, Yamane K. Involvement of fluctuating high blood pressure in the enlargement of spontaneous intracerebral hematoma. Neurol Med Chir (Tokyo). 2001. 41:300–304.12. Kazui S, Naritomi H, Yamamoto H, Sawada Y, Yamaguchi T. Enlargement of spontaneous intracerebral hemorrhage. Incidence and time course. Stroke. 1996. 27:1783–1787.13. Yang GY, Betz AL, Chenevert TL, Brunberg JA, Hoff JT. Experimenal intracerebral hemorrhage: relationship between brain edema, blood flow, and blood-brain barrier permeability in rats. J Neurosurg. 1994. 81:93–102.14. Mayer SA, Sacco RL, Shi T, Mohr JP. Neurologic deterioration in noncomatose patients with supratentorial intracerebral hemorrhage. Neurology. 1994. 44:1379–1384.15. Qureshi AI, Wilson DA, Hanley DF, Traystman RJ. Pharmacologic reduction of mean arterial pressure does not adversely affect regional cerebral blood flow and intracranial pressure in experimental intracerebral hemorrhage. Crit Care Med. 1999. 27:965–971.16. Dandapani BK, Suzuki S, Kelley RE, Reyes-Iglesias Y, Duncan RC. Relation between blood pressure and outcome in intracerebral hemorrhage. Stroke. 1995. 26:21–24.17. Wallace JD, Levy L. Blood pressure after stroke. JAMA. 1981. 246:2177–2180.18. Halpern NA, Goldberg M, Neely C, Sladen RN, Goldberg JS, Floyd J, Gabrielson G, Greenstein RJ. Postoperative hypertension: a multicenter, prospective, randomized comparison between intravenous incardipine and sodium nitroprusside. Crit Care Med. 1992. 20:1637–1643.19. Ropper AH, Zervas NT. Cerebral blood flow after experimental basal ganglia hemorrhage. Ann Neurol. 1982. 11:266–271.20. Nath FP, Kelley PT, Jenkins A, Mendelow AD, Graham DI, Teasdale GM. Effects of experimental intracerebral hemorrhage on blood flow, capillary permeability, and histochemistry. J Neurosurg. 1987. 66:555–562.21. Qureshi AI, Harris-Lane P, Kirmani JF, Ahmed S, Jacob M, Zada Y, Divani AA. Treatment of acute hypertension in patients with intracerebral hemorrhage using American Heart Association guidelines. Crit Care Med. 2006. 34:1975–1980.22. Powers WJ. Acute hypertension after stroke: the scientific basis for treatment decisions. Neurology. 1993. 43:461–467.23. Nishiyama T, Yokoyama T, Matsukawa T, Hanaoka K. Continuous Nicardipine HCl infusion to control blood pressure after evacuation of acute cerebral hemorrhage. Can J Anaesth. 2000. 47:1196–1201.24. Wallin JD, Fletcher E, Ram CV, Cook ME, Cheung DG, MacCarthy EP, TowNsend ER, Saunders E, Davis WR, Langford HG, et al. Intravenous nicardipine HCl for the treatment of severe hypertension. A double-blind, placebo-controlled multicenter trial. Arch Intern Med. 1989. 149:2662–2669.25. IV Nicardipine HCl Study Group. Efficacy and safety of intravenous Nicardipine HCl in the control of postoperative hypertension. Chest. 1991. 99:393–398.26. Powers WJ, Zazulia AR, Videen TO, Adams RE, Yundt KD, Aiyagari V, Grubb RL Jr, Diringer MN. Autoregulation of cerebral blood flow surrounding acute (2 to 22 hours) intracerebral hemorrhage. Neurology. 2001. 57:18–24.27. Abe K, Iwanaga H, Inada E. Effect of nicardipine and diltiazem on internal carotid artery blood flow velocity and local cerebral blood flow during cerebral aneurysm surgery for subarachnoid hemorrhage. J Clin Anesth. 1994. 6:99–105.28. Broderick JP, Brott TG, Tomsick T, Barsan W, Spilker J. Ultra-early evaluation of intracerebral hemorrhage. J Neurosurg. 1990. 72:195–199.29. Kothari RU, Brott T, Broderick JP, Barsan W, Sauerbeck LR, Zuccarello M, Khoury J. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996. 27:1304–1305.30. Brott T, Broderick J, Kothari R, Barsan W, Tomsick T, Sauerbeck LR, Spilker J, Duldner J, Khoury J. Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke. 1997. 28:1–5.31. Qureshi AI, Bliwise DL, Dliwise NG, Akbar MS, Uzen G, Frankel MR. Rate of 24-hour blood pressure decline and mortality after spontaneous intracerebral hemorrhage: a retrospective analysis with a random effects regression model. Crit Care Med. 1999. 27:480–485.32. Anderson CS, Huang Y, Wang JG, Arima H, Neal B, Peng B, Heeley E, Skulina C, Parsons MW, Kim JS, et al. Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT): a randomized pilot trial. Lancet Neurol. 2008. 7:391–399.33. Qureshi AI, Safdar K, Weil J, Barch C, Bliwise DL, Colohan AR, Mackay B, Frankel MR. Predictors of early deterioration and mortality in black Americans with spontaneous intracerebral hemorrhage. Stroke. 1995. 26:1764–1767.34. Fujii Y, Takeuchi S, Sasaki O, Minakawa T, Tanaka R. Multivariate analysis of predictors of hematoma enlargement in spontaneous intracerebral hemorrhage. Stroke. 1998. 29:1160–1166.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Observation on Antihypertensive Effect of Nicardipine Hydrochloride(Perdipine(R))
- Clinical Observation on Antihypertensive Effects of Nicardipine Hydrochloride(Perdipine(R))
- Nicardipine Hydrochloride Injectable Phase IV Clinical Trial-Study on the antihypertensive effect and safety of nicardipine for acute aortic dissection
- A Clinical Trial on Antihypertensive Effect of Nicardipine Hydrochloride
- Aortic Stiffness in Patients with Deep and Lobar Intracerebral Hemorrhage: Role of Antihypertensive Drugs and Statins