J Korean Med Sci.
2012 Sep;27(9):1051-1056. 10.3346/jkms.2012.27.9.1051.
Mid-term Outcomes of Total Arterial Revascularization Versus Conventional Coronary Surgery in Isolated Three-Vessel Coronary Disease
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 2Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jwlee@amc.seoul.kr
- 3Department of Thoracic and Cardiovascular Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 1782138
- DOI: http://doi.org/10.3346/jkms.2012.27.9.1051
Abstract
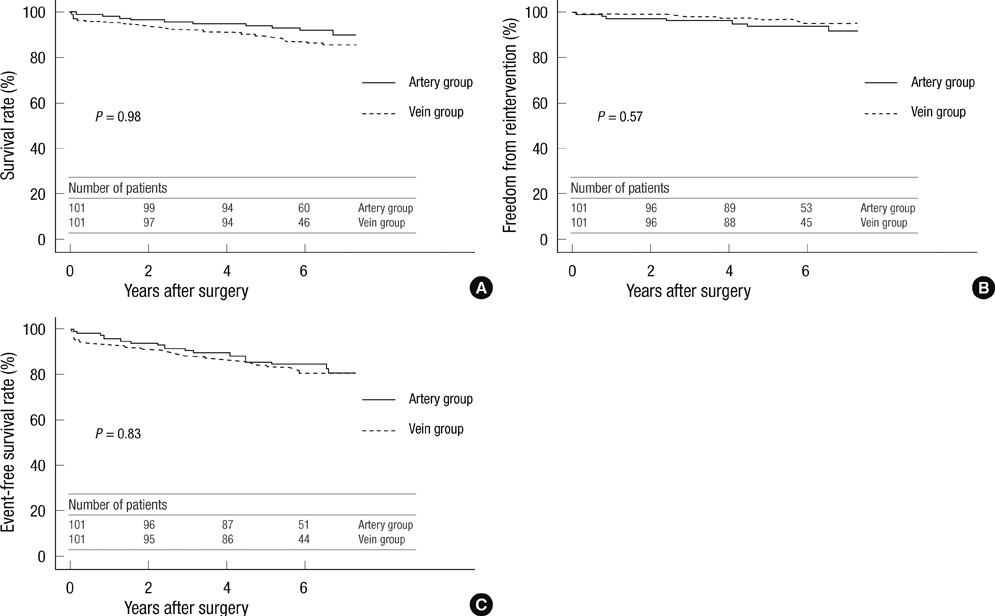
- Whether arterial conduits are superior to venous grafts in coronary artery bypassing has been debated. The aim of this study was to investigate clinical outcomes after total arterial revascularization versus conventional coronary bypassing using both arterial and venous conduits in isolated three-vessel coronary disease. Between 2003 and 2005, 503 patients who underwent isolated coronary artery bypass grafting for three-vessel coronary disease were enrolled. A total of 117 patients underwent total arterial revascularization (Artery group) whereas 386 patients were treated with arterial and venous conduits (Vein group). Major adverse outcomes (death, myocardial infarction, stroke and repeat revascularization) were compared. Clinical follow-up was complete in all patients with a mean duration of 6.1 +/- 0.9 yr. After adjustment for differences in baseline risk factors, risks of death (hazard ratio [HR] 0.96; 95% confidence interval [CI] 0.51-1.82, P = 0.90), myocardial infarction (HR 0.20, 95% CI 0.02-2.63, P = 0.22), stroke (HR 1.29, 95% CI 0.35-4.72, P = 0.70), repeat revascularization (HR 0.64, 95% CI 0.26-1.55, P = 0.32) and the composite outcomes (HR 0.83, 95% CI 0.50-1.36, P = 0.45) were similar between two groups. Since the use of veins does not increase the risks of adverse outcomes compared with total arterial revascularization, a selection of the conduit should be more liberal.
Keyword
MeSH Terms
Figure
Reference
-
1. Cameron A, Davis KB, Green G, Schaff HV. Coronary bypass surgery with internal-thoracic-artery grafts--effects on survival over a 15-year period. N Engl J Med. 1996. 334:216–219.2. Collins P, Webb CM, Chong CF, Moat NE. Radial artery versus saphenous vein patency randomized trial: five-year angiographic follow-up. Circulation. 2008. 117:2859–2864.3. Desai ND, Cohen EA, Naylor CD, Fremes SE. A randomized comparison of radial-artery and saphenous-vein coronary bypass grafts. N Engl J Med. 2004. 351:2302–2309.4. Maniar HS, Sundt TM, Barner HB, Prasad SM, Peterson L, Absi T, Moustakidis P. Effect of target stenosis and location on radial artery graft patency. J Thorac Cardiovasc Surg. 2002. 123:45–52.5. Hayward PA, Gordon IR, Hare DL, Matalanis G, Horrigan ML, Rosalion A, Buxton BF. Comparable patencies of the radial artery and right internal thoracic artery or saphenous vein beyond 5 years: results from the Radial Artery Patency and Clinical Outcomes trial. J Thorac Cardiovasc Surg. 2010. 139:60–65.6. Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy GA, Gardner TJ, Hart JC, Herrmann HC, Hillis LD, Hutter AM Jr, et al. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery). Circulation. 2004. 110:e340–e437.7. D'Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998. 17:2265–2281.8. Acar C, Ramsheyi A, Pagny JY, Jebara V, Barrier P, Fabiani JN, Deloche A, Guermonprez JL, Carpentier A. The radial artery for coronary artery bypass grafting: clinical and angiographic results at five years. J Thorac Cardiovasc Surg. 1998. 116:981–989.9. Possati G, Gaudino M, Alessandrini F, Luciani N, Trani C, Cellini C, Canosa C, Di Sciascio G. Midterm clinical and angiographic results of radial artery grafts used for myocardial revascularization. J Thorac Cardiovasc Surg. 1998. 116:1015–1021.10. Taggart DP, D'Amico R, Altman DG. Effect of arterial revascularisation on survival: a systematic review of studies comparing bilateral and single internal mammary arteries. Lancet. 2001. 358:870–875.11. Loop FD, Lytle BW, Cosgrove DM, Stewar RW, Goormastic M, Williams GW, Golding LA, Gill CC, Taylor PC, Sheldon WC, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med. 1986. 314:1–6.12. Khot UN, Friedman DT, Pettersson G, Smedira NG, Li J, Ellis SG. Radial artery bypass grafts have an increased occurrence of angiographically severe stenosis and occlusion compared with left internal mammary arteries and saphenous Vein Grafts. Circulation. 2004. 109:2086–2091.13. Weinschelbaum EE, Macchia A, Caramutti VM, Machain HA, Raffaelli HA, Favaloro MR, Favaloro RR, Dulbecco EA, Abud JA, Laurentiis MD, et al. Myocardial revascularization with radial and mammary arteries: initial and mid-term results. Ann Thorac Surg. 2000. 70:1378–1383.14. Tatoulis J, Buxton BF, Fuller JA. The right internal thoracic artery: the forgotten conduit--5,766 patients and 991 angiograms. Ann Thorac Surg. 2011. 92:9–17.15. Navia D, Vrancic M, Vaccarino G, Piccinini F, Raich H, Florit S, Thierer J. Total arterial off-pump coronary revascularization using bilateral internal thoracic arteries in triple-vessel disease: Surgical technique and clinical outcomes. Ann Thorac Surg. 2008. 86:524–530.16. Taggart DP, Altman DG, Gray AM, Lees B, Nuqara F, Yu LM, Campbell H, Flather M. Randomized trial to compare bilateral vs. single internal mammary coronary artery bypass grafting: 1-year results of the Arterial Revascularisation Trial (ART). Eur Heart J. 2010. 31:2470–2481.17. Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease. Pathogenesis, predisposition and prevention. Circulation. 1998. 97:916–931.18. Campeau L. Lipid lowering and coronary bypass graft surgery. Curr Opin Cardiol. 2000. 15:395–399.19. Kulik A, Ruel M. Statins and coronary artery bypass graft surgery: preoperative and postoperative efficacy and safety. Expert Opin Drug Sa. 2009. 8:559–571.20. Shukla N, Angelini GD, Wan I, Jeremy JY. Potential role of nitroaspirins in the treatment of vein graft failure. Ann Thorac Surg. 2003. 75:1437–1442.21. Wan S, Yim A, Shukla N, Johnson JL, Angelini GD, Jeremy JY. Nitric oxide donating aspirin (NCX 4016) inhibits neointimal thickening in a pig model of saphenous vein into carotid artery interposition grafting: a comparison with aspirin and morpholinosydnonimine. J Thorac Cardiovasc Surg. 2007. 134:1033–1039.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of the Surgical Treatment of Ischemic Heart Disease
- Bilateral versus Single Internal Thoracic Artery Grafting Strategies Supplemented by Radial Artery Grafting
- The Right Gastroepiploic Artery Graft for Coronary Artery Bypass Grafting: A 30-Year Experience
- Percutaneous coronary intervention in patients with multi-vessel coronary artery disease: a focus on physiology
- Angiographic Evaluation of Occlusive Coronary Arterial Disease