Korean J Radiol.
2009 Jun;10(3):207-216. 10.3348/kjr.2009.10.3.207.
Radiological Findings of Extensively Drug-Resistant Pulmonary Tuberculosis in Non-AIDS Adults: Comparisons with Findings of Multidrug-Resistant and Drug-Sensitive Tuberculosis
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea. kyungs.lee@samsung.com
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea.
- KMID: 1779447
- DOI: http://doi.org/10.3348/kjr.2009.10.3.207
Abstract
OBJECTIVE
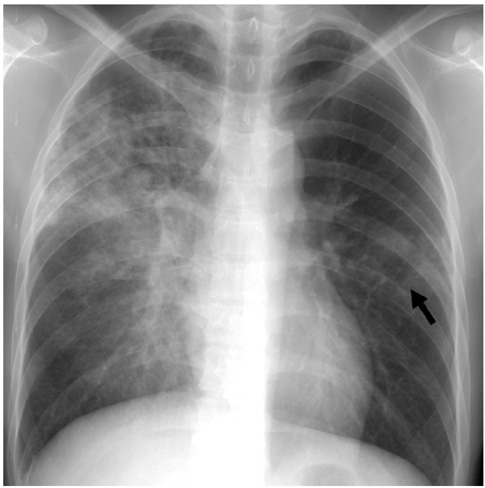
This study was designed to describe the radiological findings of extensively drug-resistant (XDR) pulmonary tuberculosis (TB) and to compare the observed findings with findings of drug-sensitive (DS) and non-XDR multidrug-resistant (MDR) TB in non-AIDS patients. MATERIALS AND METHODS: From September 1994 to December 2007, 53 MDR TB patients (M:F = 32:21; mean age, 38 years) and 15 XDR TB non-AIDS patients (M:F = 8:7; mean age, 36 years) were enrolled in the study. All of the MDR TB patients had received no treatment or less than one month of anti-TB treatment. In addition, all XDR TB patients received either no anti-TB treatment or only first-line anti-TB drugs. In addition, 141 consecutive DS TB patients (M:F = 79:62; mean age, 51 years) were also enrolled in the study for comparison. Chest radiograph, CT and demographic findings were reviewed and were compared among the three patient groups. RESULTS: For patients with XDR TB, the most frequent radiographic abnormalities were nodules (15 of 15 patients, 100%), reticulo-nodular densities (11 of 15, 73%), consolidation (9 of 15, 60%) and cavities (7 of 15, 47%) that were located mainly in the upper and middle lung zones. As seen on radiographs, significant differences were found for the frequency of nodules and ground-glass opacity lesions (all p < 0.001) (more frequent in DS TB patients than in MDR and XDR TB patients). For the use of CT, significant differences (more frequent in MDR and XDR TB patients) were found for the frequency of multiple cavities, nodules and bronchial dilatation (p = 0.001 or p < 0.001). Patients with MDR TB and XDR TB were younger as compared to patients with DS TB (p < 0.001). Imaging findings were not different between patients with MDR TB and XDR TB. CONCLUSION: By observation of multiple cavities, nodules and bronchial dilatation as depicted on CT in young patients with acid-fast bacilli (AFB) positive sputum, the presence of MDR TB or XDR TB rather than DS TB can be suggested. There is no significant difference in imaging findings between patients with XDR TB and MDR TB.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Aged, 80 and over
Drug Resistance, Bacterial
Drug Resistance, Multiple, Bacterial
Female
Humans
Image Processing, Computer-Assisted/methods
Lung/drug effects/radiography
Male
Middle Aged
Observer Variation
Retrospective Studies
Tomography, X-Ray Computed/methods
Tuberculosis, Multidrug-Resistant/*radiography
Tuberculosis, Pulmonary/*drug therapy/*radiography
Young Adult
Figure
Reference
-
1. Extensively drug-resistant tuberculosis (XDR-TB): recommendations for prevention and control. Wkly Epidemiol Rec. 2006. 81:430–432.2. Gandhi NR, Moll A, Sturm AW, Pawinski R, Govender T, Lalloo U, et al. Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet. 2006. 368:1575–1580.3. Centers for Disease Control and Prevention (CDC). Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs-worldwide, 2000-2004. MMWR Morb Mortal Wkly Rep. 2006. 55:301–305.4. Raviglione MC, Smith IM. XDR tuberculosis-implications for global public health. N Engl J Med. 2007. 356:656–659.5. Kim HR, Hwang SS, Kim HJ, Lee SM, Yoo CG, Kim YW, et al. Impact of extensive drug resistance on treatment outcomes in non-HIV-infected patients with multidrug-resistant tuberculosis. Clin Infect Dis. 2007. 45:1290–1295.6. Migliori GB, Besozzi G, Girardi E, Kliiman K, Lange C, Toungoussova OS, et al. Clinical and operational value of the extensively drug-resistant tuberculosis definition. Eur Respir J. 2007. 30:623–626.7. Kwon YS, Kim YH, Suh GY, Chung MP, Kim H, Kwon OJ, et al. Treatment outcomes for HIV-uninfected patients with multidrug-resistant and extensively drug-resistant tuberculosis. Clin Infect Dis. 208. 47:496–502.8. Mitnick CD, Shin SS, Seung KJ, Rich ML, Atwood SS, Furin JJ, et al. Comprehensive treatment of extensively drug-resistant tuberculosis. N Engl J Med. 2008. 359:563–574.9. Keshavjee S, Gelmanova IY, Farmer PE, Mishustin SP, Strelis AK, Andreev YG, et al. Treatment of extensively drug-resistant tuberculosis in Tomsk, Russia: a retrospective cohort study. Lancet. 2008. 372:1403–1409.10. Kim DH, Kim HJ, Park SK, Kong SJ, Kim YS, Kim TH, et al. Treatment outcomes and long-term survival in patients with extensively drug-resistant tuberculosis. Am J Respir Crit Care Med. 2008. 178:1075–1082.11. Shah NS, Pratt R, Armstrong L, Robinson V, Castro KG, Cegielski JP. Extensively drug-resistant tuberculosis in the United States, 1993-2007. JAMA. 2008. 300:2153–2160.12. Choi JC, Lim SY, Suh GY, Chung MP, Kim H, Kwon OJ, et al. Drug resistance rates of Mycobacterium tuberculosis at a private referral center in Korea. J Korean Med Sci. 2007. 22:677–681.13. Jeon CY, Hwang SH, Min JH, Prevots DR, Goldfeder LC, Lee H, et al. Extensively drug-resistant tuberculosis in South Korea: risk factors and treatment outcomes among patients at a tertiary referral hospital. Clin Infect Dis. 2008. 46:42–49.14. Chung MJ, Lee KS, Koh WJ, Kim TS, Kang EY, Kim SM, et al. Drug-sensitive tuberculosis, multidrug-resistant tuberculosis, and nontuberculous mycobacterial pulmonary disease in nonAIDS adults: comparisons of thin-section CT findings. Eur Radiol. 2006. 16:1934–1941.15. Eng J. Sample size estimation: how many individuals should be studied? Radiology. 2003. 227:309–313.16. Fleiss JL. Statistical methods for rates and proportions. 1981. New York, NY: Wiley;45.17. Hansell DM, Bankier AA, MacMahon H, McLoud TC, Muller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008. 246:697–722.18. Fishman JE, Sais GJ, Schwartz DS, Otten J. Radiographic findings and patterns in multidrug-resistant tuberculosis. J Thorac Imaging. 1998. 13:65–71.19. Greenberg SD, Frager D, Suster B, Walker S, Stavropoulos C, Rothpearl A. Active pulmonary tuberculosis in patients with AIDS: spectrum of radiographic findings (including a normal appearance). Radiology. 1994. 193:115–119.20. Lessnau KD, Gorla M, Talavera W. Radiographic findings in HIV-positive patients with sensitive and resistant tuberculosis. Chest. 1994. 106:687–689.21. Kim HC, Goo JM, Lee HJ, Park SH, Park CM, Kim TJ, et al. Multidrug-resistant tuberculosis versus drug-sensitive tuberculosis in human immunodeficiency virus-negative patients: computed tomography features. J Comput Assist Tomogr. 2004. 28:366–371.22. Geng E, Kreiswirth B, Burzynski J, Schluger NW. Clinical and radiographic correlates of primary and reactivation tuberculosis: a molecular epidemiology study. JAMA. 2005. 293:2740–2745.23. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea (2005.1-2005.12). 2006.24. Bai GH, Park YK, Choi YW, Bai JI, Kim HJ, Chang CL, et al. Trend of anti-tuberculosis drug resistance in Korea, 1994-2004. Int J Tuberc Lung Dis. 2007. 11:571–576.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Medical Management of Drug-Resistant Tuberculosis
- Current status of drug-resistant tuberculosis and its treatment
- Medical Treatment of Pulmonary Multidrug-Resistant Tuberculosis
- Drug Resistance Patterns of Multidrug- and Extensively Drug-Resistant Tuberculosis in Korea: Amplification of Resistance to Oral Second-line Drugs
- Extensively Drug Resistant-Tuberculosis, XDR-TB