Korean J Radiol.
2007 Jun;8(3):249-253. 10.3348/kjr.2007.8.3.249.
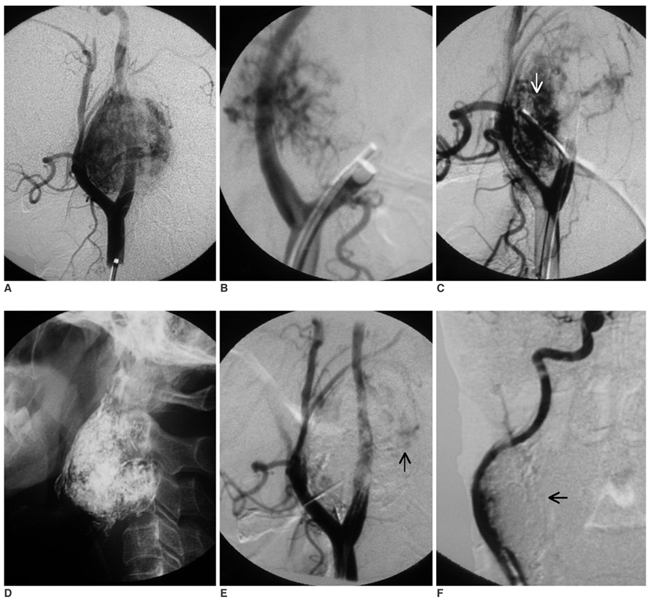
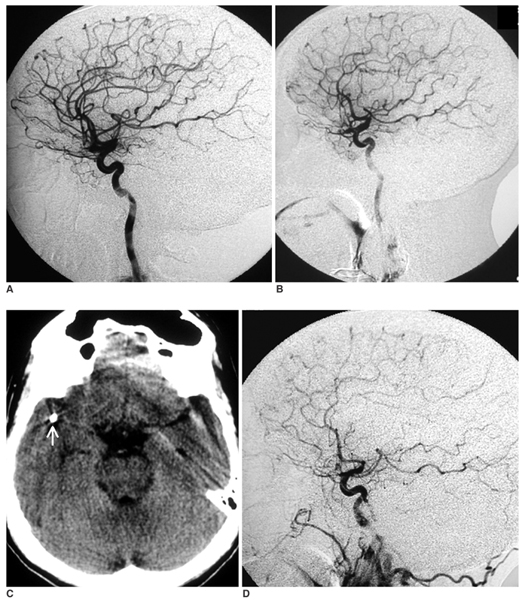
Stroke from Delayed Embolization of Polymerized Glue Following Percutaneous Direct Injection of a Carotid Body Tumor
- Affiliations
-
- 1Department of Imaging Sciences and Interventional Radiology, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, Kerala, India. b_krish1@yahoo.co.in
- KMID: 1779443
- DOI: http://doi.org/10.3348/kjr.2007.8.3.249
Abstract
- A 52-year-old male with right carotid body tumor underwent direct percutaneous glue (n-butylcyanoacrylate [NBCA]) embolization. Several hours later, he developed left hemiparesis from embolization of the polymerized glue cast. Migration of glue during percutaneous tumor embolization is presumed to occur only in the liquid state, which may lead to stroke or cranial nerve deficits. To the best of our knowledge, this is the first report of delayed glue embolization from a treated hypervascular tumor of the head and neck.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A safer endovascular technique for pre-operative embolization of juvenile nasopharyngeal angiofibroma: avoiding the pitfalls of external carotid artery – internal carotid artery anastomoses
David Rosenbaum-Halevi, Victor Lopez-Rivera, Ali Turkmani, Aditya Sanzgiri, Hussein A. Zeineddine, Amber Luong, Peng Roc Chen
J Cerebrovasc Endovasc Neurosurg. 2020;22(2):97-105. doi: 10.7461/jcen.2020.22.2.97.
Reference
-
1. Casasco A, Herbreteau D, Houdart E, George B, Tran Ba Huy P, Deffresne D, et al. Devascularization of craniofacial tumors by percutaneous tumor puncture. AJNR Am J Neuroradiol. 1994. 15:1233–1239.2. George B, Casasco A, Deffrennes D, Houdart E. Intratumoral embolization of intracranial and extracranial tumors: technical note. Neurosurgery. 1994. 35:771–773.3. Valavanis A. Preoperative embolization of the head and neck: indications, patient selection, goals, and precautions. AJNR Am J Neuroradiol. 1986. 7:943–952.4. Abud DG, Mounayer C, Benndorf G, Piotin M, Spelle L, Moret J. Intratumoral injection of cyanoacrylate glue in head and neck paragangliomas. AJNR Am J Neuroradiol. 2004. 25:1457–1462.5. Horowitz M, Whisnant RE, Jungreis C, Snyderman C, Levy EI, Kassam A. Temporary balloon occlusion and ethanol injection for preoperative embolization of carotid-body tumor. Ear Nose Throat J. 2002. 81:536–538. 540542 passim6. Lonser RR, Heiss JD, Oldfield EH. Tumor devascularization by intratumoral ethanol injection during surgery. Technical note. J Neurosurg. 1998. 88:923–924.7. Harman M, Etlik O, Unal O. Direct percutaneous embolization of a carotid body tumor with n-butyl cyanoacrylate: an alternative method to endovascular embolization. Acta Radiol. 2004. 45:646–648.8. Liang Y, Wang D, Huang W, Ling F, Liu Y, Lu F. Direct intratumoral embolization of hypervascular tumors of the head and neck. Chin Med J. 2003. 116:616–619.9. Casasco A, Houdart E, Biondi A, Jhaveri HS, Herbreteau D, Aymard A, et al. Major complications of percutaneous embolization of skull-base tumors. AJNR Am J Neuroradiol. 1999. 20:179–181.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous N-Butyl Cyanoacrylate Embolization of a Pancreatic Pseudoaneurysm after Failed Attempts of Transcatheter Embolization
- Carotid Body Tumors
- Carotid Artery Reconstruction during the Resection of Carotid Body Tumor: A case report
- A Case of Pseudoaneurysm of the Supraorbital Artery Treated with Percutaneous Glue Embolization
- A Case of Carotid Body Tumor: Case Report