Korean J Pain.
2013 Jan;26(1):65-71. 10.3344/kjp.2013.26.1.65.
Scrambler Therapy for Patients with Cancer Pain: Case Series
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea. jymoon0901@gmail.com
- KMID: 1779027
- DOI: http://doi.org/10.3344/kjp.2013.26.1.65
Abstract
- More than 80% of cancer patients experience cancer pain. Among them, more than 50% experience moderate to severe pain. To control cancer pain, a variety of methods have been used, including medications and nerve blocks. In some patients, however, it is impossible to perform nerve blocks due to caner metastasis into the epidural space, while in other patients, opioid dose escalation is impossible due to opioid side effects; thus, cancer pain management is difficult. Scrambler therapy is a novel approach for pain control that uses EKG-like pads, which are applied above and below the site of pain. Scrambler therapy synthesizes 16 different types of nerve action potentials that provide "non-pain" information via cutaneous nerves. The advantages of this treatment are that it is non-invasive and safe and has no significant side effects. In this case series, we report the treatment results of using scrambler therapy in three cancer patients with intractable pain.
MeSH Terms
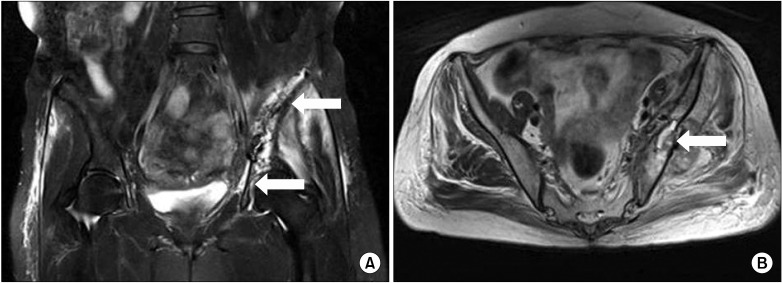
Figure
Reference
-
1. Breivik H, Cherny N, Collett B, de Conno F, Filbet M, Foubert AJ, et al. Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol. 2009; 20:1420–1433. PMID: 19244085.
Article2. Von Roenn JH, Cleeland CS, Gonin R, Hatfield AK, Pandya KJ. Physician attitudes and practice in cancer pain management. A survey from the Eastern Cooperative Oncology Group. Ann Intern Med. 1993; 119:121–126. PMID: 8099769.
Article3. Zenz M, Zenz T, Tryba M, Strumpf M. Severe undertreatment of cancer pain: a 3-year survey of the German situation. J Pain Symptom Manage. 1995; 10:187–191. PMID: 7629412.
Article5. Li SL, Wang DX, Ma D. Epidural hematoma after neuraxial blockade: a retrospective report from China. Anesth Analg. 2010; 111:1322–1324. PMID: 20705781.6. Mertes N, Goeters C, Bantel C, Gullotta F, Van Aken H. Brain death during anesthesia due to undiagnosed meningeal carcinomatosis of gastric adenocarcinoma. Anesthesiology. 1999; 90:630–631. PMID: 9952174.
Article7. Marineo G, Iorno V, Gandini C, Moschini V, Smith TJ. Scrambler therapy may relieve chronic neuropathic pain more effectively than guideline-based drug management: results of a pilot, randomized, controlled trial. J Pain Symptom Manage. 2012; 43:87–95. PMID: 21763099.
Article8. Smith TJ, Coyne PJ, Parker GL, Dodson P, Ramakrishnan V. Pilot trial of a patient-specific cutaneous electrostimulation device (MC5-A Calmare®) for chemotherapy-induced peripheral neuropathy. J Pain Symptom Manage. 2010; 40:883–891. PMID: 20813492.
Article9. Marineo G. Untreatable pain resulting from abdominal cancer: new hope from biophysics? JOP. 2003; 4:1–10. PMID: 12555009.10. Sabato AF, Marineo G, Gatti A. Scrambler therapy. Minerva Anestesiol. 2005; 71:479–482. PMID: 16012423.11. de Leon-Casasola OA. Spinal cord and peripheral nerve stimulation techniques for neuropathic pain. J Pain Symptom Manage. 2009; 38:S28–S38. PMID: 19671469.
Article12. Foletti A, Durrer A, Buchser E. Neurostimulation technology for the treatment of chronic pain: a focus on spinal cord stimulation. Expert Rev Med Devices. 2007; 4:201–214. PMID: 17359225.
Article13. Jensen MP. A neuropsychological model of pain: research and clinical implications. J Pain. 2010; 11:2–12. PMID: 19595637.
Article14. Nathan PW, Wall PD. Treatment of post-herpetic neuralgia by prolonged electric stimulation. Br Med J. 1974; 3:645–647. PMID: 4425789.
Article15. Niv D, Maltsman-Tseikhin A, Lang E. Postherpetic neuralgia: what do we know and where are we heading? Pain Physician. 2004; 7:239–247. PMID: 16868598.16. Harke H, Gretenkort P, Ladleif HU, Rahman S. Spinal cord stimulation in sympathetically maintained complex regional pain syndrome type I with severe disability. A prospective clinical study. Eur J Pain. 2005; 9:363–373. PMID: 15979016.
Article17. Harke H, Gretenkort P, Ladleif HU, Koester P, Rahman S. Spinal cord stimulation in postherpetic neuralgia and in acute herpes zoster pain. Anesth Analg. 2002; 94:694–700. PMID: 11867400.
Article18. Kumar K, Taylor RS, Jacques L, Eldabe S, Meglio M, Molet J, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007; 132:179–188. PMID: 17845835.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Scrambler (Calmare) Therapy for Intractable Chronic Pain
- Clinical Experiences on the Effect of Scrambler Therapy for Patients with Postherpetic Neuralgia
- Transcutaneous neurostimulatory treatment for peripheral polyneuropathy induced by hypereosinophilic syndrome - A case report -
- TBR2-immunopsitive unipolar brush cells are associated with ectopic zebrin II-immunoreactive Purkinje cell clusters in the cerebellum of scrambler mice
- Systemic fungal infection following effective pain relief with high-dose steroid therapy for terminal cancer pain: A case report