Yonsei Med J.
2009 Dec;50(6):838-844. 10.3349/ymj.2009.50.6.838.
Diagnostic Value of 3D Fast Low-Angle Shot Dynamic MRI of Breast Papillomas
- Affiliations
-
- 1Department of Radiology, The Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Korea. ejsonrd@yuhs.ac
- 2Department of General Surgery, The Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1777100
- DOI: http://doi.org/10.3349/ymj.2009.50.6.838
Abstract
- PURPOSE
To evaluate the value of breast MRI in analysis of papillomas of the breast.
MATERIALS AND METHODS
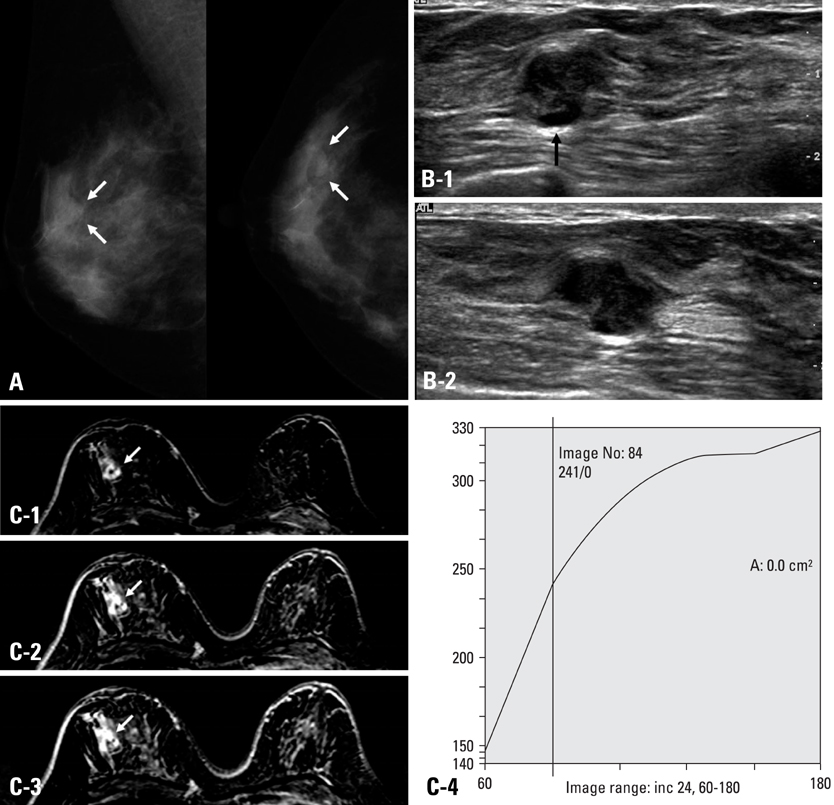
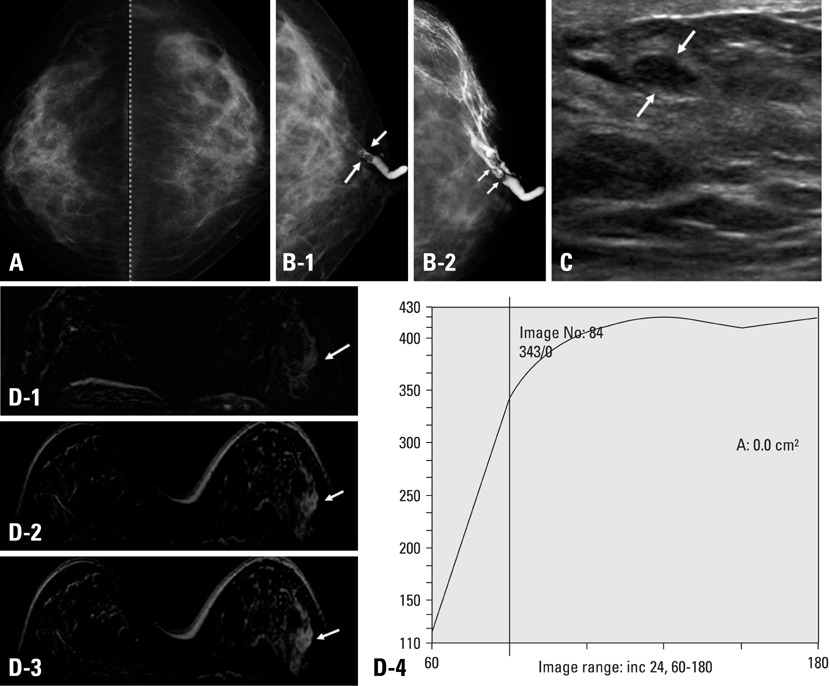
From 1996 to 2004, 94 patients underwent surgery due to papillomas of the breast. Among them, 21 patients underwent 3D fast low angle shot (FLASH) dynamic breast MRI. Eight masses were palpable and 11 of 21 patients had nipple discharge. Two radiologists indifferently analyzed the location, size of the lesions and shape, margin of the masses, multiplicity and ductal relation. The MRI findings were categorized according to breast imaging reporting and data system (BI-RADS) lexicon. The amount and pattern of enhancement and associated findings were also evaluated according to BI-RADS. We then compared the MRI findings with galactography, mammography and breast ultrasonography (US) and examined histopathologic correlation.
RESULTS
On breast MRI, the lesion size was 0.4-1.59 cm, and 18 patients showed subareolar location. On 4.25 cm (mean 1.54) dynamic enhanced images, imaging findings showed mass (n = 10), intracystic mass (n = 3), focus (n = 5), ductal enhancement (n = 2), and segmental enhancement (n = 1). In cases of the masses, the shapes of the masses were round (n = 4), lobulated (n = 3), and irregular (n = 6), and margins were circumscribed (n = 6), microlobulated (n = 5), and indistinct (n = 2). The enhancement patterns were homogeneous enhancement (n = 7), heterogeneous (n = 3) or rim enhancement (n = 3).
CONCLUSION
The contrast enhanced dynamic breast MRI was highly sensitive for diagnosis of breast papillomas. MRI could play a key role in the pre-operative work-up for multiple papillomas and papillomatosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Al Sarakbi W, Worku D, Escobar PF, Mokbel K. Breast papillomas: current management with a focus on a new diagnostic and therapeutic modality. Int Semin Surg Oncol. 2006. 3:1.
Article2. Francis A, England D, Rowlands D, Bradley S. Breast papilloma: mammogram, ultrasound and MRI appearances. Breast. 2002. 11:394–397.
Article3. Cardenosa G, Eklund GW. Benign papillary neoplasms of the breast: mammographic findings. Radiology. 1991. 181:751–755.
Article4. Piccoli CW, Feig SA, Vala MA. Breast imaging case of the day. Benign intraductal papilloma with focal atypical papillomatous hyperplasia. Radiographics. 1998. 18:783–786.
Article5. Pisano ED, Braeuning MP, Burke E. Diagnosis please. Case 8: solitary intraductal papilloma. Radiology. 1999. 210:795–798.6. Woods ER, Helvie MA, Ikeda DM, Mandell SH, Chapel KL, Adler DD. Solitary breast papilloma: comparison of mammographic, galactographic, and pathologic findings. AJR Am J Roentgenol. 1992. 159:487–491.
Article7. Krämer SC, Rieber A, Görich J, Aschoff AJ, Tomczak R, Merkle EM, et al. Diagnosis of papillomas of the breast: value of magnetic resonance mammography in comparison with galactography. Eur Radiol. 2000. 10:1733–1736.
Article8. Daniel BL, Gardner RW, Birdwell RL, Nowels KW, Johnson D. Magnetic resonance imaging of intraductal papilloma of the breast. Magn Reson Imaging. 2003. 21:887–892.
Article9. Oyama T, Koerner FC. Noninvasive papillary proliferations. Semin Diagn Pathol. 2004. 21:32–41.10. Dietz JR, Crowe JP, Grundfest S, Arrigain S, Kim JA. Directed duct excision by using mammary ductoscopy in patients with pathologic nipple discharge. Surgery. 2002. 132:582–587.
Article11. Carter D. Intraductal papillary tumours of the breast: a study of 78 cases. Cancer. 1977. 39:1689–1692.
Article12. Haagensen CD, Bodain C, Haagensen DE. Breast carcinoma risk and detection. 1981. Philadelphia: Saunders;146.13. Dupont WD, Page DL. Risk factors for breast cancer in women with proliferative breast disease. N Engl J Med. 1985. 312:46–51.
Article14. Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW. Ten-year risk of false positive screening mammograms and clinical breast examinations. N Engl J Med. 1998. 338:1089–1096.
Article15. Okazaki A, Hirata K, Okazaki M, Svane G, Azavedo E. Nipple discharge disorders: current diagnostic management and the role of fiber-ductoscopy. Eur Radiol. 1999. 9:583–590.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Value of 3D-Gradient Echo Dynamic Contrast Enhanced MRI in Breast Cancer
- Estimation of Pulmonary Motion in Healthy Subjects and Patients with Intrathoracic Tumors Using 3D-Dynamic MRI: Initial Results
- Diagnostic Value of MRI in the T Staging of Colorectal Carcinoma
- MR Imaging of Portal System: Comparison between True-Fast Imaging with Steady State Precession(FISP) and Enhanced Fast Low Angle Shot(FLASH) Imaging
- 3D Whole-Heart Coronary MR Angiography at 1.5T in Healthy Volunteers: Comparison between Unenhanced SSFP and Gd-Enhanced FLASH Sequences