Korean Circ J.
2010 Jan;40(1):31-35. 10.4070/kcj.2010.40.1.31.
The Recent Surgical Result of Total Anomalous Pulmonary Venous Return
- Affiliations
-
- 1Department of Pediatrics, Sejong General Hospital, Bucheon, Korea. prelud15@nate.com
- 2Department of Cardiac Surgery, Sejong General Hospital, Bucheon, Korea.
- KMID: 1776303
- DOI: http://doi.org/10.4070/kcj.2010.40.1.31
Abstract
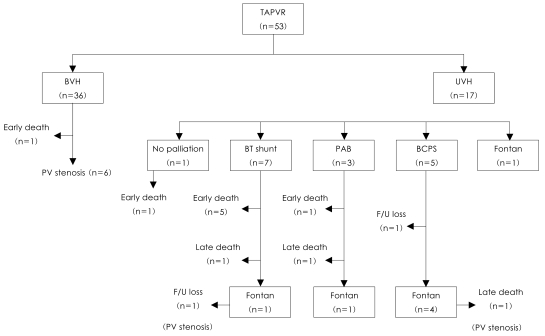
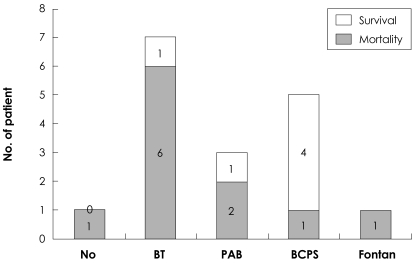
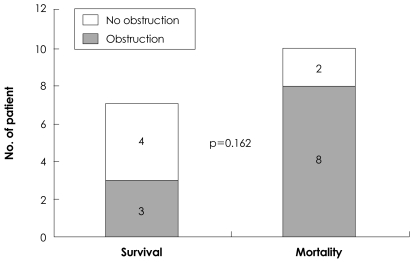
- BACKGROUND AND OBJECTIVES
Recent surgical results from total anomalous pulmonary venous return (TAPVR) are reported to have improved; however, mortality and morbidity are still high in the univentricles. This review was performed in order to demonstrate surgical results from TAPVR for recent years in a single institute. SUBJECTS AND METHODS: A total of 53 patients with TAPVR underwent surgery between January 2000 and December 2008. Preoperative anatomy and hemodynamics were evaluated by 2-dimensional echocardiogram. We reviewed medical records on preoperative management, age, and body weight at time of surgery, postoperative mortality, and pulmonary venous obstruction. RESULTS: The study included 36 biventricle patients and 17 univentricle patients. Median age and weight at time of surgery were 26 days and 3.5 kg, respectively. During the mean follow up period of 48.2 months, a total of 11 deaths and 8 early deaths occurred. Postoperative pulmonary venous stenosis occurred in 8 patients. Among 36 biventricle patients, mortality occurred in 1 patient and postoperative pulmonary venous stenosis occurred in 6 patients. No statistical significances were observed between postoperative pulmonary venous stenosis and other factors. Among 17 univentricule patients, mortality was 10, including 7 early deaths, and postoperative pulmonary venous stenosis occurred in 2 patients. Combined palliations were modified Blalock-Taussig (BT) shunts in 7, pulmonary artery banding (PAB) in 3, bidirectional cavopulmonary shunt in 5, and the Fontan procedure in 1. The highest mortality was recorded in patients with a modified BT shunt (85.7%) and next in patients with PAB (66.6%). Mortality was not related to anatomy of TAPVR, nor preoperative obstruction, but with significant age and weight at time of surgery. CONCLUSION: Despite improvement in operative results from TAPVR, surgery in univentricles is highly risky, especially with low weight and early age, with concomitant palliation.
Keyword
MeSH Terms
Figure
Reference
-
1. Kirshbom PM, Myung RJ, Gaynor JW, et al. Preoperative pulmonary venous obstruction affects long-term outcome for survivors of total anomalous pulmonary venous connection repair. Ann Thorac Surg. 2002; 74:1616–1620. PMID: 12440618.2. Caldarone CA, Najm HK, Kadletz M, et al. Surgical management of total anomalous pulmonary venous drainage: impact of coexisting cardiac anomalies. Ann Thorac Surg. 1998; 66:1521–1526. PMID: 9875745.3. Hancock Friesen CL, Zurakowski D, Thiagarajan RR, et al. Total anomalous pulmonary venous connection: an analysis of current management strategies in a single institution. Ann Thorac Surg. 2005; 79:596–606. PMID: 15680843.4. Gaynor JW, Collins MH, Rychik J, Gaughan JP, Spray TL. Long-term outcome of infants with single ventricle and total anomalous pulmonary venous connection. J Thorac Cardiovasc Surg. 1999; 117:506–514. PMID: 10047654.5. Heinemann MK, Hanley FL, Van Praagh S, et al. Total anomalous pulmonary venous drainage in newborns with visceral heterotaxy. Ann Thorac Surg. 1994; 57:88–91. PMID: 8279925.6. Chu MA, Choi BH, Choi HJ, et al. Clinical features and results of recent total anomalous pulmonary venous connection: experience in a university hospital (clinical study of total anomalous pulmonary venous connection). Korean J Pediatr. 2009; 52:194–198.7. Lee JR, Kim CY, Kim HK, Lee JS, Kim YJ, Rho JR. Surgical results and risk factor analysis of the patients with single ventricle associated with total anomalous pulmonary venous connection. Korean J Thorac Cardiovasc Surg. 2002; 35:862–870.8. Bando K, Turrentine MW, Ensing GJ, et al. Surgical management of total anomalous pulmonary venous connection: thirty-year trends. Circulation. 1996; 94(9 Suppl):II12–II16. PMID: 8901712.9. Caldarone CA, Behrendt DM. Total anomalous pulmonary venous drainage associated with complex cardiac anatomy. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2000; 3:142–152. PMID: 11486192.10. Karamlou T, Gurofsky R, Al Sukhni E, et al. Factors associated with mortality and reoperation in 377 children with total anomalous pulmonary venous connection. Circulation. 2007; 115:1591–1598. PMID: 17353446.11. Song JY, Yoon YS. Long-term clinical study of total anomalous pulmonary venous return. J Korean Pediatr Soc. 2000; 43:229–235.12. van de Wal HJ, Hamilton DI, Godman MJ, Harinck E, Lacquet LK, van Oort A. Pulmonary venous obstruction following correction for total anomalous pulmonary venous drainage: a challenge. Eur J Cardiothorac Surg. 1992; 6:545–549. PMID: 1389237.13. Ando M, Takahashi Y, Kikuchi T. Total anomalous pulmonary venous connection with dysmorphic pulmonary vein: a risk for postoperative pulmonary venous obstruction. Interact Cardiovasc Thorac Surg. 2004; 3:557–561. PMID: 17670310.14. Devaney EJ, Ohye RG, Bove EL. Pulmonary vein stenosis following repair of total anomalous pulmonary venous connection. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2006; 9:51–55. PMID: 16638548.15. Lamb RK, Qureshi SA, Wilkinson JL, Arnold R, West CR, Hamilton DI. Total anomalous pulmonary venous drainage: seventeen-year surgical experience. J Thorac Cardiovasc Surg. 1988; 96:368–375. PMID: 3411981.16. Morales DL, Braud BE, Booth JH, et al. Heterotaxy patients with total anomalous pulmonary venous return: improving surgical results. Ann Thorac Surg. 2006; 82:1621–1628. PMID: 17062215.17. Kim SJ, Han MY, Lee JY, et al. Follow up of patients with total anomalous pulmonary venous return in right atrial isomerism. J Korean Pediatr Soc. 2000; 43:1451–1457.18. Yamaki S, Tsunemoto M, Shimada M, et al. Quantitative analysis of pulmonary vascular disease in total anomalous pulmonary venous connection in sixty infants. J Thorac Cardiovasc Surg. 1992; 104:728–735. PMID: 1513162.19. Jenkins KJ, Sanders SP, Orav EJ, Coleman EA, Mayer JE Jr, Colan SD. Individual pulmonary vein size and survival in infants with totally anomalous pulmonary venous connection. J Am Coll Cardiol. 1993; 22:201–206. PMID: 8509542.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Surgically Corrected-Combined form of Total Anomalous Pulmonary Venous Return
- Anomalous Pulmonary Venous Return Accompanied by Normal Superior Pulmonary Veins in the Left Upper Lobe: A Case Report
- Repair of Total Anomalous Pulmonary Venous Return in Infant
- Cor Triatriatum Associated with Total Anomalous Pulmonary Venous Connection: A Rare but Plausible Combination
- Levoatriocardinal Vein Combined with Pulmonary Venous Varix Mimicking Arteriovenous Malformations: A Case Report