Korean J Gastroenterol.
2013 Jan;61(1):42-45. 10.4166/kjg.2013.61.1.42.
A Case of Acute Cholecystitis after Colonoscopy
- Affiliations
-
- 1Department of Internal Medicine, Gangneung Asan Hospital, Ulsan University College of Medicine, Gangneung, Korea. jwoojini@naver.com
- KMID: 1775786
- DOI: http://doi.org/10.4166/kjg.2013.61.1.42
Abstract
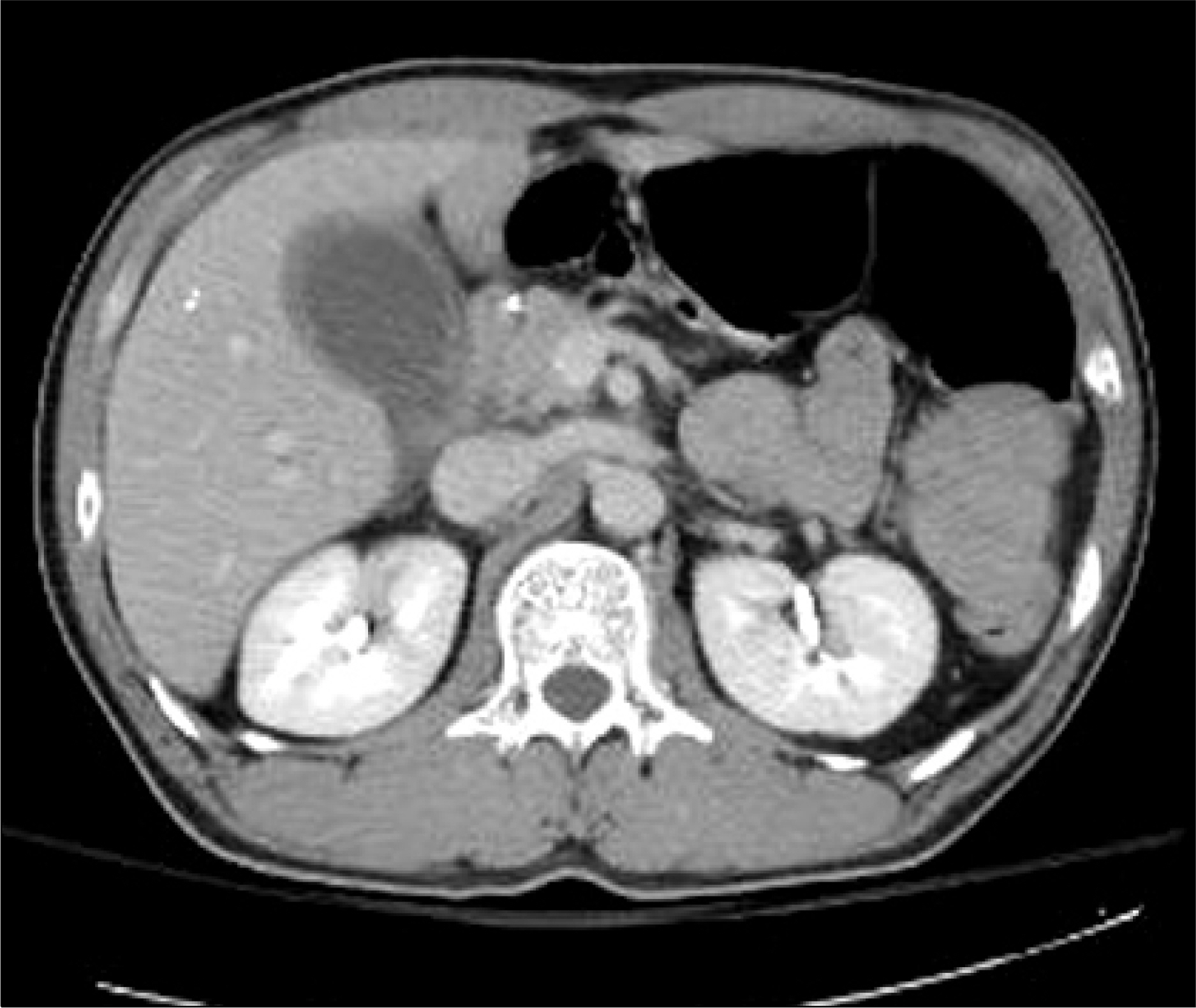
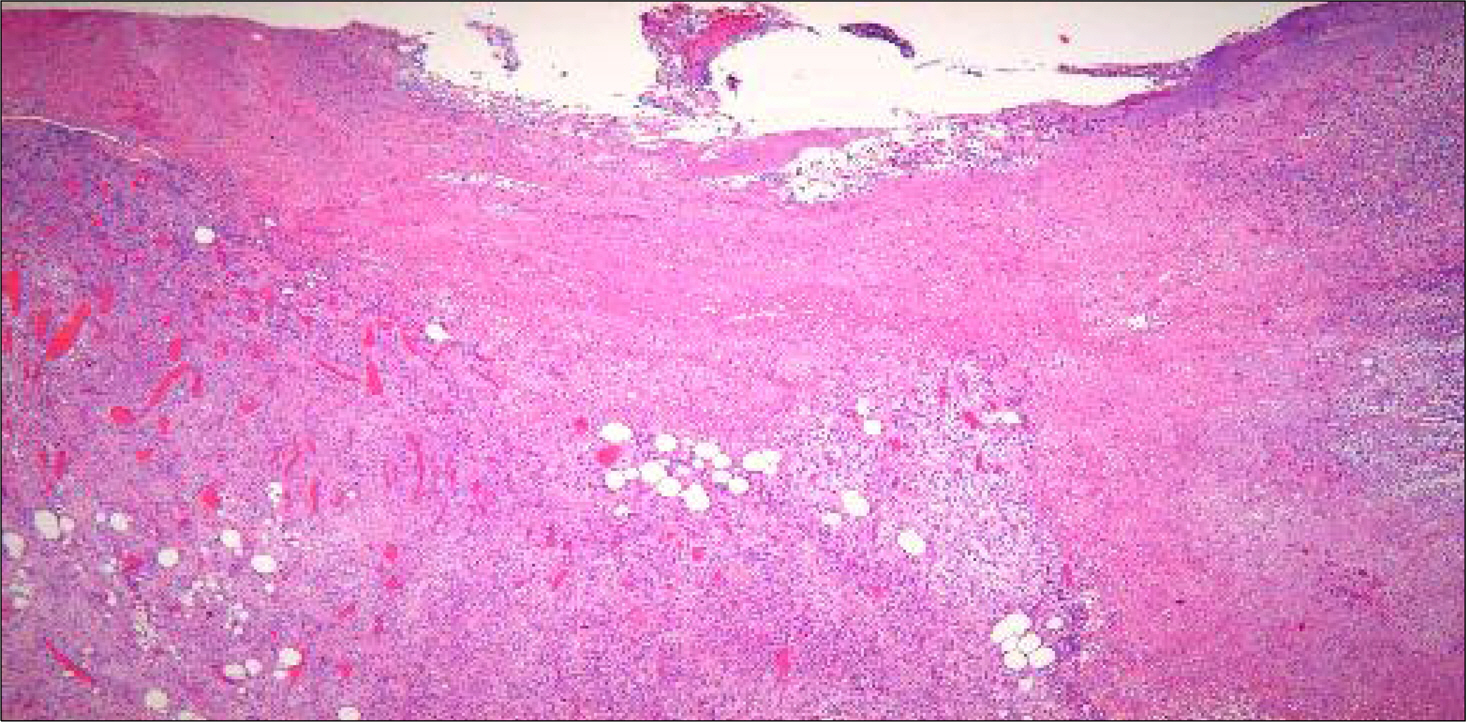
- A 43-year-old man, who received total gastrectomy five years ago for advanced gastric cancer, underwent a screening colonoscopy and abdominal CT scan. Abdominal CT scan revealed no abnormal findings. Colonoscopy revealed polyps at the rectum, which were removed by polypectomy. The patient did not complain of abdominal pain or discomfort throughout the procedure. But, he developed right upper quadrant abdominal pain on the next day after colonoscopy. Abdominal CT scan revealed the distended gallbladder with mild wall thickening and suspicious sandy stones or sludge in the gallbladder. The patient underwent an open cholecystectomy. Pathology was compatible with acute cholecystitis. We should be aware of and consider cholecystitis in the differential diagnosis for patients with abdominal pain after colonoscopy.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Rabeneck L, Paszat LF, Hilsden RJ, et al. Bleeding and perforation after outpatient colonoscopy and their risk factors in usual clinical practice. Gastroenterology. 2008; 135:1899–1906.
Article2. Ko CW, Riffle S, Shapiro JA, et al. Incidence of minor complications and time lost from normal activities after screening or surveillance colonoscopy. Gastrointest Endosc. 2007; 65:648–656.
Article3. Milman PJ, Goldenberg SP. Colonoscopy cholecystitis. Am J Gastroenterol. 2001; 96:1666.
Article4. Fernández-Martínez C, Plá-Martí V, Flors-Alandí C, Roig-Vila JV. Gangrenous cholecystitis after colonoscopy. Am J Gastroenterol. 2002; 97:1572.
Article5. Aziz F, Milman P, McNelis J. Abdominal pain after colonoscopy: can it be acute cholecystitis? Dig Dis Sci. 2007; 52:2660–2661.
Article6. Maddur H, Agrawal S, Fayad N, Chalasani N, Kahi C. Acute cholecystitis after colonoscopy: a case series. Gastrointest Endosc. 2011; 74:211–213.
Article