J Korean Surg Soc.
2010 Apr;78(4):262-266. 10.4174/jkss.2010.78.4.262.
Tips for Delayed Open Conversion in Patients with a Type III Endoleak after Endovascular Aortic Aneurysm Repair
- Affiliations
-
- 1Division of Vascular Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dikim@skku.edu
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Surgery, Kyung Hee University Medical Center, Seoul, Korea.
- KMID: 1750741
- DOI: http://doi.org/10.4174/jkss.2010.78.4.262
Abstract
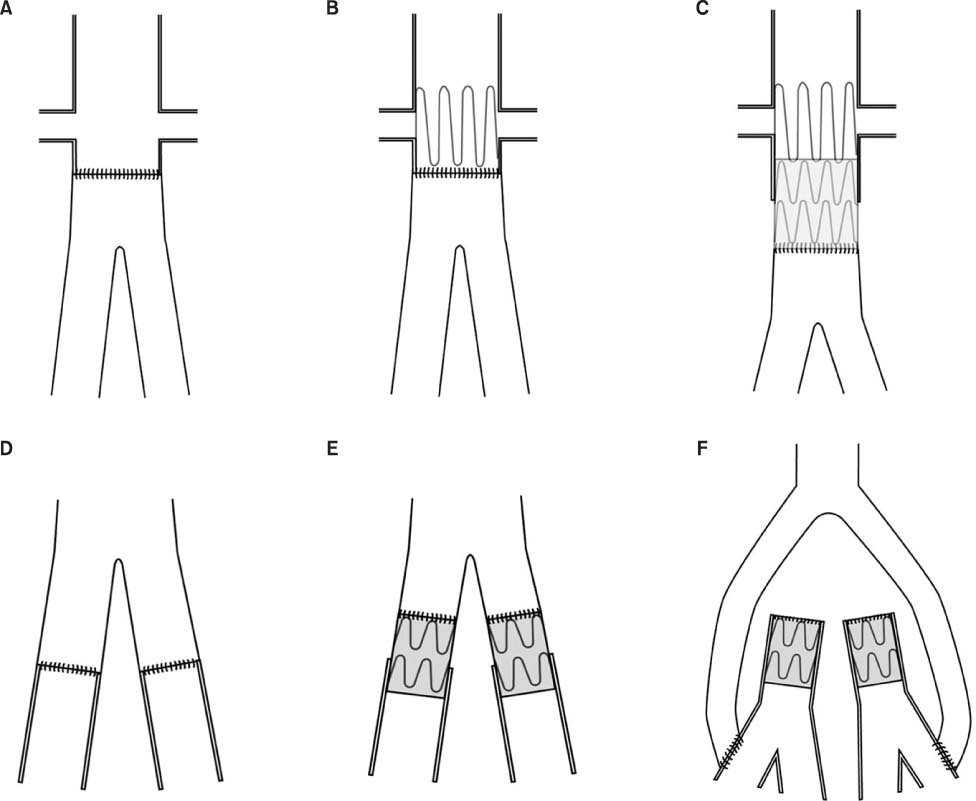
- Type III endoleak is one of the causes of secondary intervention after endovascular aortic aneurysm repair (EVAR). We report two cases of a late type III endoleak with a review of the literature. One case had a disconnected iliac limb and the other case was due to a defect of the main body fabric at the bifurcation level. Both cases were successfully treated by open conversion. Before open conversion, it should be determined how to get proximal aortic control (suprarenal vs. infrarenal and cross-clamping vs. balloon inflation). When the suprarenal aortic control is required, to reduce suprarenal clamping time, it is not necessary to remove the endograft completely. Partial endograft removal and a graft-to-graft anastomosis is an alternative, if it is well incorporated and not infected. Making a plan for delayed open conversion should be individualized according to the type and status of the endograft and the vascular anatomy.
MeSH Terms
Figure
Reference
-
1. Giles KA, Pomposelli F, Hamdan A, Wyers M, Jhaveri A, Schermerhorn ML. Decrease in total aneurysm-related deaths in the era of endovascular aneurysm repair. J Vasc Surg. 2009. 49:543–551.2. Drury D, Michaels JA, Jones L, Ayiku L. Systematic review of recent evidence for the safety and efficacy of elective endovascular repair in the management of infrarenal abdominal aortic aneurysm. Br J Surg. 2005. 92:937–946.3. Lyden SP, McNamara JM, Sternbach Y, Illig KA, Waldman DL, Green RM. Technical considerations for late removal of aortic endografts. J Vasc Surg. 2002. 36:674–678.4. Verzini F, Cao P, De Rango P, Parlani G, Xanthopoulos D, Iacono G, et al. Conversion to open repair after endografting for abdominal aortic aneurysm: causes, incidence and results. Eur J Vasc Endovasc Surg. 2006. 31:136–142.5. Lee WA, Huber TS, Seeger JM. Late type III endoleak from graft erosion of an Excluder stent graft: a case report. J Vasc Surg. 2006. 44:183–185.6. Brown KE, Heyer KS, Matsumura JS, Eskandari MK. Late type III endoleak and graft failure of an Ancure stent-graft. J Vasc Interv Radiol. 2008. 19:1506–1508.7. Bauer EP, Redaelli C, von Segesser LK, Turina MI. Ruptured abdominal aortic aneurysms: predictors for early complications and death. Surgery. 1993. 114:31–35.8. Jimenez JC, Moore WS, Quinones-Baldrich WJ. Acute and chronic open conversion after endovascular aortic aneurysm repair: a 14-year review. J Vasc Surg. 2007. 46:642–647.9. McArthur C, Teodorescu V, Eisen L, Morrissey N, Faries P, Hollier L, et al. Histopathologic analysis of endovascular stent grafts from patients with aortic aneurysms: Does healing occur? J Vasc Surg. 2001. 33:733–738.10. Jacobowitz GR, Lee AM, Riles TS. Immediate and late explantation of endovascular aortic grafts: the endovascular technologies experience. J Vasc Surg. 1999. 29:309–316.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Endovascular Treatment of Delayed Type Ib Endoleak with Aortic Rupture after Endovascular Repair of Abdominal Aortic Aneurysm
- Late Type 3b Endoleak Mimicking Type 2 Endoleak after Endovascular Aortic Aneurysm Repair
- Delayed Type III Endoleak Caused by Fabric Erosion after Endovascular Repair of an Abdominal Aortic Aneurysm
- Endovascular Reintervention for Stent-Graft Dislocation after Open Surgical Conversion for Thoracoabdominal Aortic Aneurysm Treated by Thoracic Endovascular Aortic Repair
- Off-the-Shelf, Hybrid, Innominate Chimney Thoracic Endovascular Aneurysm Repair for Treatment of Mycotic Thoracic Aortic Aneurysm: A Case Report