Clin Orthop Surg.
2011 Sep;3(3):254-257. 10.4055/cios.2011.3.3.254.
Chronic Osteomyelitis of the Lumbar Transverse Process
- Affiliations
-
- 1Department of Orthopedics, Myongji Hospital, Kwandong University College of Medicine, Jecheon, Korea.
- 2Department of Orthopaedic Surgery, Cheju Halla General Hospital, Jeju, Korea. schstk27@hanmail.net
- KMID: 1743918
- DOI: http://doi.org/10.4055/cios.2011.3.3.254
Abstract
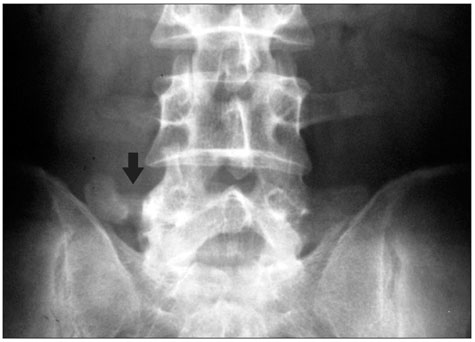
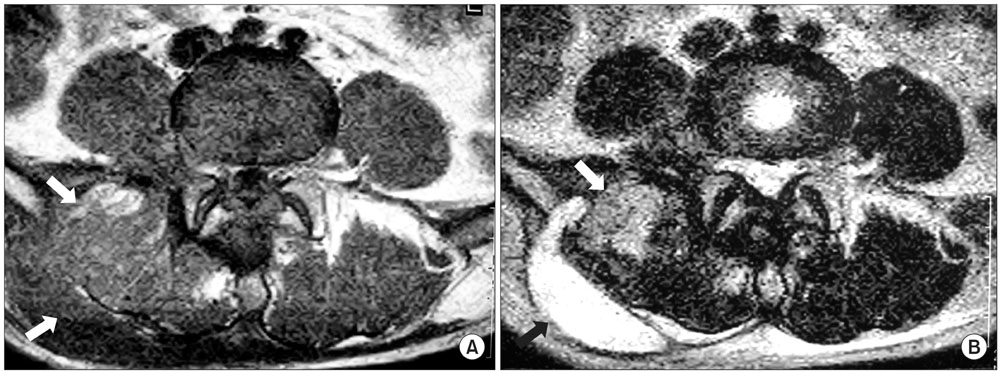
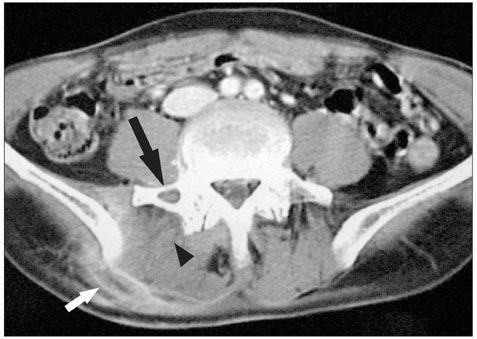
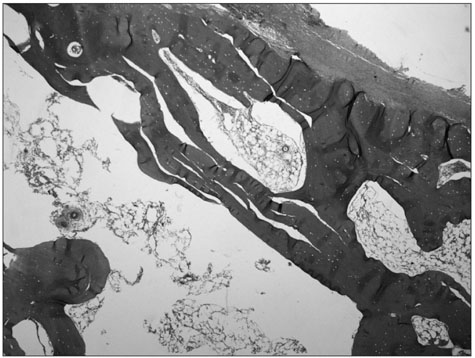
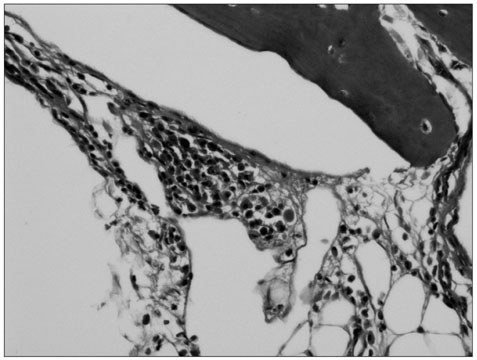
- Pyogenic spondylitis involving only the posterior element of a vertebra is rare. To the best of our knowledge, there have been no reports of osteomyelitis of the transverse process. We report here on a 45-year-old male with a one month history of swelling associated with lower back pain. The magnetic resonance imaging showed a paraspinal soft tissue mass, and computed tomography revealed a fine osteolytic lesion in the right transverse process of the 5th lumbar spine, and this was all consistent with chronic osteomyelitis. A mixed staphylococcal infection was identified. Open drainage, resection of the transverse process and intravenous injection of anti-staphylococcal antibiotics resolved the back pain and reduced the erythrocyte sedimentation rate to normal. Pyogenic osteomyelitis of the transverse process is extremely rare, which can cause a misdiagnosis or a delayed diagnosis. Careful consideration of this disease is needed when evaluating patients who complain of back pain.
Keyword
MeSH Terms
Figure
Reference
-
1. Calderone RR, Larsen JM. Overview and classification of spinal infections. Orthop Clin North Am. 1996. 27(1):1–8.
Article2. Buoncristiani AM, McCullen G, Shin AY, Bathgate B, Akbarnia BA. An unusual cause of low back pain: osteomyelitis of the spinous process. Spine (Phila Pa 1976). 1998. 23(7):839–841.3. Ehara S, Khurana JS, Kattapuram SV. Pyogenic vertebral osteomyelitis of the posterior elements. Skeletal Radiol. 1989. 18(3):175–178.
Article4. Garcia A Jr, Grantham SA. Hematogenous pyogenic vertebral osteomyelitis. J Bone Joint Surg Am. 1960. 42(3):429–436.
Article5. Batson OV. The vertebral vein system: Caldwell lecture, 1956. Am J Roentgenol Radium Ther Nucl Med. 1957. 78(2):195–212.6. Wiley AM, Trueta J. The vascular anatomy of the spine and its relationship to pyogenic vertebral osteomyelitis. J Bone Joint Surg Br. 1959. 41(4):796–809.
Article7. Sapico FL. Microbiology and antimicrobial therapy of spinal infections. Orthop Clin North Am. 1996. 27(1):9–13.
Article8. Tali ET. Spinal infections. Eur J Radiol. 2004. 50(2):120–133.
Article9. King DM, Mayo KM. Subacute haematogenous osteomyelitis. J Bone Joint Surg Br. 1969. 51(3):458–463.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiological Study of the Transverse Processes of the Lumbar Spine
- Chronic Recurrent Multifocal Osteomyelitis: A Case Report
- Osteomyelitis Resulting from Chronic Septic Olecranon Bursitis: Report of Two Cases
- Treatment of Chronic Osteomyelitis by Transplantation of Autogenous Omentum with Microvascular Anastomosis
- Congenital Osseus Bridging of Lumbar Transverse Processes