J Korean Soc Radiol.
2014 Sep;71(3):111-119. 10.3348/jksr.2014.71.3.111.
Incidental Thyroid Lesions Detected on 18F-Fluorodeoxyglucose Positron Emission Tomography/CT in Patients with Non-Thyroidal Cancer: Clinical Implications and the Value of Ultrasound
- Affiliations
-
- 1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jhshin11@skku.edu
- 2Department of Radiology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 3Department of Nuclear Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1736475
- DOI: http://doi.org/10.3348/jksr.2014.71.3.111
Abstract
- PURPOSE
To evaluate the clinical implications of subsequent ultrasound (US) for incidental thyroid lesions (ITLs) detected on positron emission tomography/computed tomography (PET/CT) in patients with non-thyroidal cancer.
MATERIALS AND METHODS
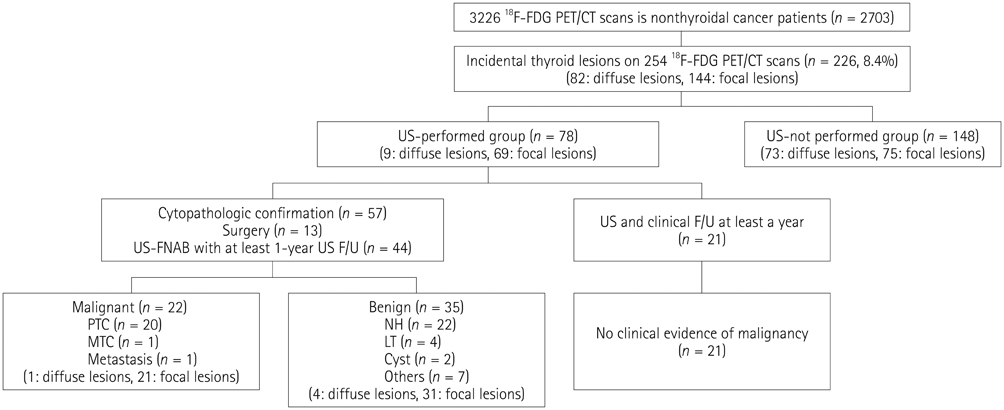
We retrospectively searched for ITLs in 2703 patients with non-thyroidal cancer on 3226 PET/CT examinations. We divided the patients into two groups: US-performed and US-not performed groups. Diagnostic performance of US in detecting malignancy was analyzed according to the PET/CT findings.
RESULTS
The incidence of ITLs on PET/CT in patients with non-thyroidal cancer was 8.4% (226/2703). Death rate from disease and stage were not significantly different between the groups. The malignant rate of ITLs that had cytopathology was 39% (22/57). All malignancies were primary thyroid cancers except for one metastasis. Overall diagnostic performance of US was 87% sensitivity, 66% specificity, 66% positive predictive value (PPV), and 89% negative predictive value (NPV). The diagnostic performance of US according to the PET/CT findings was probable benign on PET/CT (n = 9): 100% specificity, 100% NPV; suspicious malignant on PET/CT (n = 22): 75% sensitivity, 90% specificity, 90% PPV, 75% NPV; and undetermined on PET/CT (n = 26): 100% sensitivity, 94% specificity, 91% PPV, 100% NPV.
CONCLUSION
ITLs did not affect the prognosis of patients with non-thyroidal cancer whether subsequent US was performed or not. Subsequent US may be unnecessary for ITLs with probable benign findings on PET/CT.
MeSH Terms
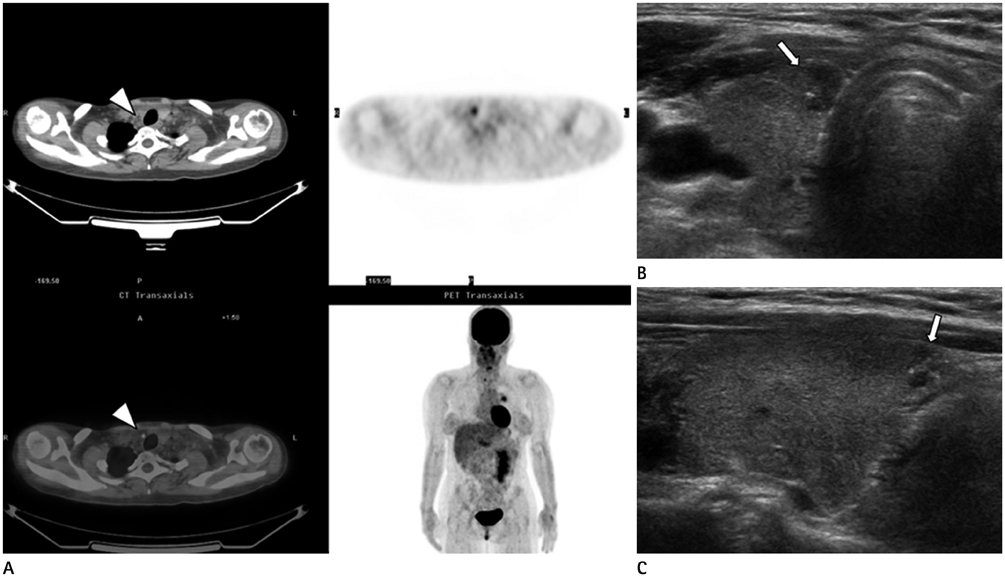
Figure
Reference
-
1. Shetty SK, Maher MM, Hahn PF, Halpern EF, Aquino SL. Significance of incidental thyroid lesions detected on CT: correlation among CT, sonography, and pathology. AJR Am J Roentgenol. 2006; 187:1349–1356.2. Bae JS, Chae BJ, Park WC, Kim JS, Kim SH, Jung SS, et al. Incidental thyroid lesions detected by FDG-PET/CT: prevalence and risk of thyroid cancer. World J Surg Oncol. 2009; 7:63.3. Kang BJ, O JH, Baik JH, Jung SL, Park YH, Chung SK. Incidental thyroid uptake on F-18 FDG PET/CT: correlation with ultrasonography and pathology. Ann Nucl Med. 2009; 23:729–737.4. Kwak JY, Kim EK, Yun M, Cho A, Kim MJ, Son EJ, et al. Thyroid incidentalomas identified by 18F-FDG PET: sonographic correlation. AJR Am J Roentgenol. 2008; 191:598–603.5. Deandreis D, Al Ghuzlan A, Auperin A, Vielh P, Caillou B, Chami L, et al. Is (18)F-fluorodeoxyglucose-PET/CT useful for the presurgical characterization of thyroid nodules with indeterminate fine needle aspiration cytology? Thyroid. 2012; 22:165–172.6. Choi JY, Lee KS, Kim HJ, Shim YM, Kwon OJ, Park K, et al. Focal thyroid lesions incidentally identified by integrated 18F-FDG PET/CT: clinical significance and improved characterization. J Nucl Med. 2006; 47:609–615.7. Moon WJ, Baek JH, Jung SL, Kim DW, Kim EK, Kim JY, et al. Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J Radiol. 2011; 12:1–14.8. Chen YK, Ding HJ, Chen KT, Chen YL, Liao AC, Shen YY, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for cancer screening in healthy subjects. Anticancer Res. 2005; 25:1421–1426.9. Cohen MS, Arslan N, Dehdashti F, Doherty GM, Lairmore TC, Brunt LM, et al. Risk of malignancy in thyroid incidentalomas identified by fluorodeoxyglucose-positron emission tomography. Surgery. 2001; 130:941–946.10. Kim SJ, Kim BH, Jeon YK, Kim SS, Kim IJ. Limited diagnostic and predictive values of dual-time-point 18F FDG PET/CT for differentiation of incidentally detected thyroid nodules. Ann Nucl Med. 2011; 25:347–353.11. Are C, Hsu JF, Schoder H, Shah JP, Larson SM, Shaha AR. FDG-PET detected thyroid incidentalomas: need for further investigation? Ann Surg Oncol. 2007; 14:239–247.12. Rheingold SR, Neugut AI, Meadows AT. Secondary cancers: incidence, risk factors, and management. In : Kufe DW, Holland JF, Frei E, editors. Cancer medicine. 6th ed. Hamilton, ON: BC Decker;2003. p. 2623.13. de Geus-Oei LF, Pieters GF, Bonenkamp JJ, Mudde AH, Bleeker-Rovers CP, Corstens FH, et al. 18F-FDG PET reduces unnecessary hemithyroidectomies for thyroid nodules with inconclusive cytologic results. J Nucl Med. 2006; 47:770–775.14. Kang KW, Kim SK, Kang HS, Lee ES, Sim JS, Lee IG, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for metastasis evaluation and cancer screening in healthy subjects. J Clin Endocrinol Metab. 2003; 88:4100–4104.15. Kim TY, Kim WB, Ryu JS, Gong G, Hong SJ, Shong YK. 18F-fluorodeoxyglucose uptake in thyroid from positron emission tomogram (PET) for evaluation in cancer patients: high prevalence of malignancy in thyroid PET incidentaloma. Laryngoscope. 2005; 115:1074–1078.16. Pagano L, Samà MT, Morani F, Prodam F, Rudoni M, Boldorini R, et al. Thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography with CT (FDG-PET/CT): clinical and pathological relevance. Clin Endocrinol (Oxf). 2011; 75:528–534.17. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.18. Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedüs L, et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and EuropeanThyroid Association Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules. Endocr Pract. 2010; 16:Suppl 1. 1–43.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Meaning of Incidental Thyroid Uptake on F-18 FDG PET-CT
- Lymphocytic Thyroiditis Presenting as a Focal Uptake on 18F-Fluorodeoxyglucose Positron Emission Tomography: A Case Report
- US Findings of Secondary Breast Lymphoma Detected by PET/CT
- Supraclavicular Lymph Node Metastasis from Various Malignancies: Assessment with 18F-Fluorodeoxyglucose Positron Emission Tomography/CT, Contrast-Enhanced CT and Ultrasound
- Perirenal 18F-FDG Uptake in a Patient with a Pheochromocytoma