J Korean Med Sci.
2014 Mar;29(3):405-410. 10.3346/jkms.2014.29.3.405.
Clinicopathologic Analysis of Pituitary Adenoma: A Single Institute Experience
- Affiliations
-
- 1Department of Pathology, Seoul National University Hospital and Seoul National University College of Medicine, Seoul, Korea. shparknp@snu.ac.kr
- 2Department of Neurosurgery, Seoul National University Hospital and Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Neuroradiology, Seoul National University Hospital and Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Industrial Engineering, Ajou University, Suwon, Korea.
- 5Neuroscience Institute, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1734929
- DOI: http://doi.org/10.3346/jkms.2014.29.3.405
Abstract
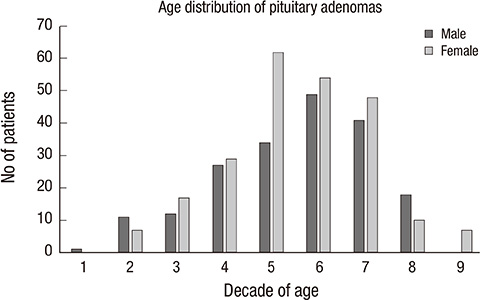
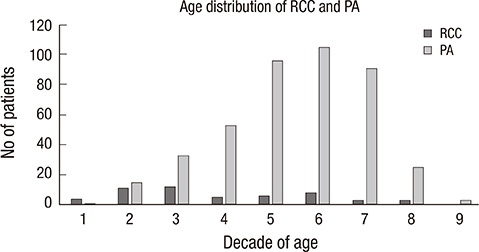
- Pituitary adenoma (PA) is a common benign neuroendocrine tumor; however, the incidence and proportion of hormone-producing PAs in Korean patients remain unknown. Authors analyzed 506 surgically resected and pathologically proven pituitary lesions of the Seoul National University Hospital from 2006 to 2011. The lesions were categorized as: PAs (n = 422, 83.4%), Rathke's cleft cysts (RCCs) (n = 54, 10.6%), inflammatory lesions (n = 8, 1.6%), meningiomas (n = 4), craniopharyngiomas (n = 4), granular cell tumors (n = 1), metastatic renal cell carcinomas (n = 2), germinomas (n = 1), ependymomas (n = 1), and unsatisfactory specimens (n = 9, 1.8%). PAs were slightly more prevalent in women (M: F = 1:1.17) with a mean age of 48.8 yr (9-80 yr). Immunohistochemical analysis revealed that prolactin-producing PAs (16.6%) and growth hormone-producing adenomas (9.2%) were the most common functional PAs. Plurihormonal PAs and nonfunctioning (null cell) adenomas were found in 14.9% and 42.4% of patients with PAs, respectively. The recurrence rate of PAs was 11.1%, but nearly 0% for the remaining benign lesions such as RCCs. 25.4% of patients with PAs were treated by gamma-knife after surgery due to residual tumors or regrowth of residual tumor. In conclusion, the pituitary lesions and the proportions of hormone-producing PAs in Korean patients are similar to those of previous reports except nonfunctioning (null cell) PAs, which are unusually frequent.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Epidemiology of Functioning Pituitary Adenomas
Sang Ouk Chin
Endocrinol Metab. 2020;35(2):237-242. doi: 10.3803/EnM.2020.35.2.237.
Reference
-
1. Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML, McCutcheon IE. The prevalence of pituitary adenomas: a systematic review. Cancer. 2004; 101:613–619.2. Nilsson B, Gustavasson-Kadaka E, Bengtsson BA, Jonsson B. Pituitary adenomas in Sweden between 1958 and 1991: incidence, survival, and mortality. J Clin Endocrinol Metab. 2000; 85:1420–1425.3. Daly AF, Burlacu MC, Livadariu E, Beckers A. The epidemiology and management of pituitary incidentalomas. Horm Res. 2007; 68:195–198.4. Fernandez A, Karavitaki N, Wass JA. Prevalence of pituitary adenomas: a community-based, cross-sectional study in Banbury (Oxfordshire, UK). Clin Endocrinol (Oxf). 2010; 72:377–382.5. Daly AF, Tichomirowa MA, Beckers A. The epidemiology and genetics of pituitary adenomas. Best Pract Res Clin Endocrinol Metab. 2009; 23:543–554.6. Arafah BM, Nasrallah MP. Pituitary tumors: pathophysiology, clinical manifestations and management. Endocr Relat Cancer. 2001; 8:287–305.7. Krysiak R, Okopień B, Korzekwa M. Atypical pituitary tumors. Pol Merkur Lekarski. 2012; 32:323–328.8. Chanson P, Brochier S. Non-functioning pituitary adenomas. J Endocrinol Invest. 2005; 28:93–99.9. Hemminki K, Försti A, Ji J. Incidence and familial risks in pituitary adenoma and associated tumors. Endocr Relat Cancer. 2007; 14:103–109.10. Raappana A, Koivukangas J, Ebeling T, Pirilä T. Incidence of pituitary adenomas in Northern Finland in 1992-2007. J Clin Endocrinol Metab. 2010; 95:4268–4275.11. Fernández-Balsells MM, Murad MH, Barwise A, Gallegos-Orozco JF, Paul A, Lane MA, Lampropulos JF, Natividad I, Perestelo-Pérez L, Ponce de León-Lovatón PG, et al. Natural history of nonfunctioning pituitary adenomas and incidentalomas: a systematic review and metaanalysis. J Clin Endocrinol Metab. 2011; 96:905–912.12. Caputo C, Sutherland T, Farish S, McNeill P, Ng KW, Inder WJ. Gender differences in presentation and outcome of nonfunctioning pituitary macroadenomas. Clin Endocrinol (Oxf). 2013; 78:564–570.13. Norberg L, Johansson R, Rasmuson T. Pituitary adenomas in northern Sweden: a study on therapy choices and the risk of second primary tumours. Clin Endocrinol (Oxf). 2008; 68:780–785.14. Murad MH, Fernández-Balsells MM, Barwise A, Gallegos-Orozco JF, Paul A, Lane MA, Lampropulos JF, Natividad I, Perestelo-Pérez L, Ponce de León-Lovatón PG, et al. Outcomes of surgical treatment for nonfunctioning pituitary adenomas: a systematic review and meta-analysis. Clin Endocrinol (Oxf). 2010; 73:777–791.15. Terada T, Kovacs K, Stefaneanu L, Horvath E. Incidence, pathology, and recurrence of pituitary adenomas: study of 647 unselected surgical cases. Endocr Pathol. 1995; 6:301–310.16. Paluzzi A, Fernandez-Miranda JC, Tonya Stefko S, Challinor S, Snyderman CH, Gardner PA. Endoscopic endonasal approach for pituitary adenomas: a series of 555 patients. Pituitary. 2013; doi: 10.1007/s11102-013-0502-4.