Yonsei Med J.
2005 Jun;46(3):408-413. 10.3349/ymj.2005.46.3.408.
The Relationship between Maximal Urethral Closure Pressure and Functional Urethral Length in Anterior Vaginal Wall Prolapse Patients According to Stage and Age
- Affiliations
-
- 1Department of Obstetrics and Gynecology and the Institute of Women's Life Science, Yonsei University College of Medicine, Seoul, Korea. swbai@yumc. yonsei.ac.kr
- KMID: 1734077
- DOI: http://doi.org/10.3349/ymj.2005.46.3.408
Abstract
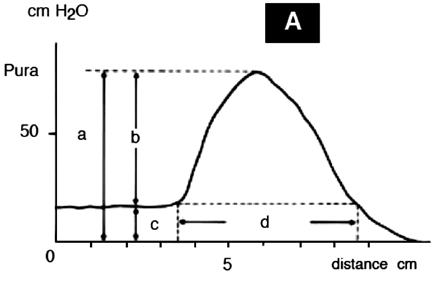
- MUCP (Maximal urethral closure pressure) is known to be increased in patients with vaginal wall prolapse due to the mechanical obstruction of the urethra. However, urethral function following reduction has not yet been completely elucidated. Predicting postoperative urethral function may provide patients with important, additional information prior to surgery. Thus, this study was performed to evaluate the relationship between MUCP and functional urethral length (FUL) according to stage and age in anterior vaginal wall prolapse patients. 139 patients diagnosed with anterior vaginal wall prolapse at Yonsei University Medical College (YUMC) from March 1999 to May 2003 who had underwent urethral pressure profilometry following reduction were included in this study. The stage of pelvic organ prolapse (POP) was determined according to the dependent portion of the anterior vaginal wall (Aa, Ba). (By International Continence Society's POP Quantification system) Patients were divided into one of four age groups: patients in their 40s (n=13), 50s (n=53), 60s (n=54), and 70 and over (n=16). No difference in MUCP was found between the age groups. The FUL of patients in their 40s was shorter than that of patient's in their 50s and 60s. Patients were also divided into stages: stage II (n=35), stage III (n=76), and stage IV (n=25). No significant difference in MUCP was found according to stage and FUL. However, a significant difference was noted between stage III and IV as stage IV was longer. Anterior vaginal wall prolapse is known to affect urethral function due to prolapse itself, but according to our study, prolapse itself did not alter urethral function. This suggests that, regardless of age and stage, prolapse corrective surgery does not affect the urethral function.
Keyword
MeSH Terms
Figure
Reference
-
1. Thompson JD. Thompson JD, Rock JA, editors. Surgical correction of defects in pelvic support. The Linde's operative gynecology. 1997. 8th ed. Philadelphia: Lippincott-Raven Publisher;963.2. Luber KM, Boero S, Choe JY. The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol. 2001. 184:1496–1501.3. Stanton SL, Mattiasson A, Hilton P. Voiding difficulty in the female prevalence, clinical and urodynamic review. Obstet Gynecol. 1983. 61:144–147.4. Richardson DA, Bent AE, Ostergard DR. The effect of uterovaginal prolapse on urethrovesical pressure dynamics. Am J Obstet Gynecol. 1983. 146:901–905.5. Bump RC, Fantl A, Hurt G. The mechanism of urinary incontinence in women with sever uterovaginal prolapse: Results of barrier studies. Obstet Gynecol. 1988. 72:291–295.6. Rosenzweig BA, Pushkin S, Blumenfeld D, Bhatia NN. Prevalence of abnormal urodynamic test results in continent women with severe genitourinary prolapse. Obstet Gynecol. 1992. 79:539–542.7. Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996. 175:10–17.8. Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardization of terminology of lower urinary tract function. Scand J Urol Nephrol. 1988. 114:5–18.9. Menefee SA, Wall LL. Jonathan SB, editor. Incontinence, Prolapse, and disorders of the Pelvic Floor. Novak's Gynecology. 2002. 13th ed. Philadelphia: Lippincott Williams & Wilkins;685–693.10. Snooks SJ, Budenoch DF, Tiptaft RC, Swash M. Perineal nerve damage in genuine stress urinary incontinence: an electrophysiological study. Br J Urol. 1985. 57:422–426.11. Busachi P, DeGiorgio R, Santini D, Bellavia E, Perry T, Oliverio C, et al. A histological and immunohistochemical study of neuropeptide containing somatic nerves in the levator ani muscle of women with genitourinary prolapse. Acta Obstet Gynecol Scand. 1999. 78:2–5.12. Bai SW, Kang SH, Kim SK, Kim JY, Park KH. The effect of pelvic organ prolapse on lower urinary tract function. Yonsei Med J. 2003. 44:94–98.13. David G, Asnat G. Evaluation of female lower urinary tract symptoms: overview and update. Curr Opin Obstet Gynecol. 2001. 13:521–527.14. Dietz HP, Haylen BT, Vancaillie TG. Female Pelvic Organ Prolapse and Voiding Function. Int Urogynecol J. 2002. 13:284–288.15. Richard CB, J Andrew F, W Glenn H. The Mechanism of Urinary Continence in Women With Severe Uterovaginal Prolapse: Results of Barrier Studies. Obstet Gynecol. 1988. 72:291–295.16. Hann-Chorng Kuo. The Relationships of Urethral and Pelvic Floor Muscles and the Urethral Pressure Measurements in Women with Stress Urinary Incontinence. Eur Urol. 2000. 37:149–155.17. Davic AR, Alfred EB, Donald RO. The effect of uterovaginal prolapse on urethrovesical pressure dynamics. Am J Obstet Gynecol. 1983. 146:901–905.18. Mattias W, Hans DM, Christian G, Heinz K. Computer-Assisted Virtual Urethral Pressure Profile in the Assessment of Female Genuine Stress Incontinence. Obstet Gynecol. 2002. 99:69–74.19. Deborah LM, Christine AL, Joseph WH, Peter LR. The Effect of Posterior Wall Support Defects on Urodynamic Indices in Stress Urinary Incontinence. Obstet Gynecol. 1998. 91:710–714.20. Richard CB, J Andrew F, W Glenn H. The Mechanism of Urinary Continence in Women With Severe Uterovaginal Prolapse: Results of Barrier Studies. Obstet Gynecol. 1988. 72:291–295.21. Chaikin DC, Groutz A, Blaivas JG. Predicting the need for anti-incontinence surgery in continent women undergoing repair of severe urogenital prolapse. J Urol. 2000. 163:531–534.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of Stress Leak-Point Pressure and Maximal Urethral Closure Pressure in Patients with Genuine Stress Incontinence
- Adult Female Urethral Prolapse
- Characteristic Changes of Cough Urethral Pressure Profile in Stress Urinary Incontinence
- Prolapse of the Female Urethra
- Is Pressure Transmission Ratio in Genuine Stress Urinary Incontinence a Good Parameter of Success after Operation?