J Korean Acad Nurs.
2013 Feb;43(1):81-90. 10.4040/jkan.2013.43.1.81.
Structural Equation Modeling On Health-related Quality of Life in Patients with Obstructive Sleep Apnea
- Affiliations
-
- 1Samsung Medical Center, Seoul, Korea. sujungchoi@hanmail.net
- 2College of Nursing, Seoul National University, Seoul, Korea.
- KMID: 1732668
- DOI: http://doi.org/10.4040/jkan.2013.43.1.81
Abstract
- PURPOSE
This study was done to test structural equation modeling of health-related quality of life (QOL) of men with obstructive sleep apnea in order to identify parameters affecting QOL and provide guidelines for interventions and strategies to improve QOL in these patients.
METHODS
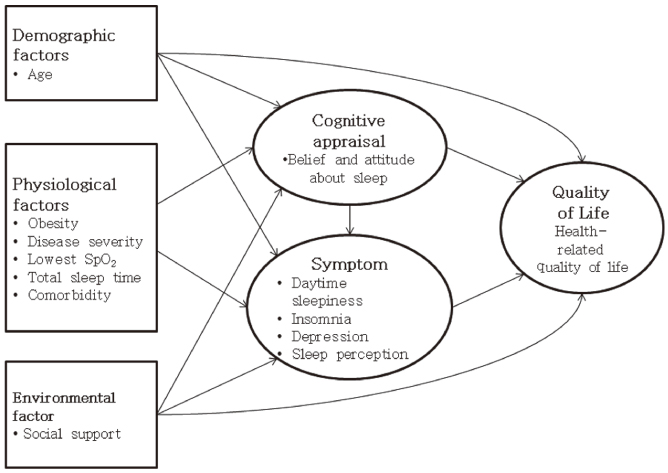
Model construction was based on 'The conceptual model of patient outcome in health-related QOL' by Wilson and Cleary, using the variables; age, physiological factors, social support, cognitive appraisal, symptoms and QOL. Participants were 201 adult male patients recruited at a tertiary university hospital in Seoul. Data were collected via questionnaires, polysomnography, and clinical records.
RESULTS
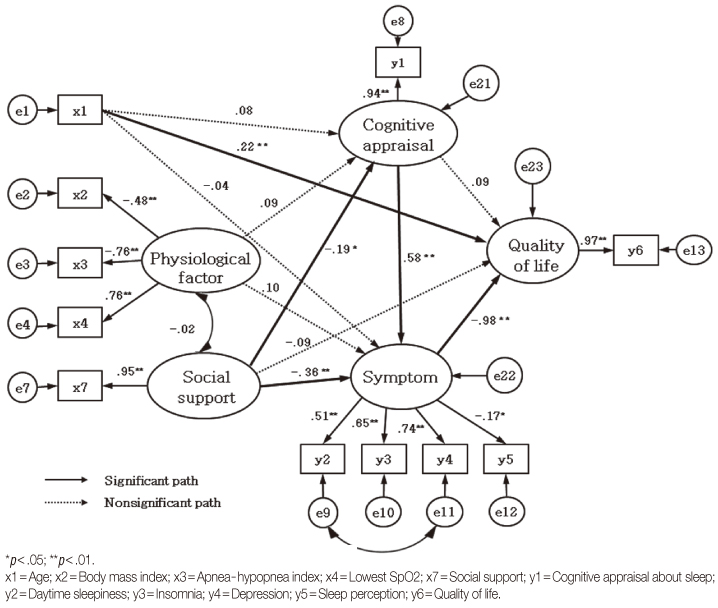
Age and symptoms directly influenced QOL. Social support and cognitive appraisal about sleep did not have a direct influence on QOL, but indirectly affected it via symptoms. QOL was lower in patients who were younger and had more severe symptoms. Symptoms were more severe for patients with lower social support and more dysfunctional cognitive appraisal. When social support was lower, cognitive appraisal was more dysfunctional.
CONCLUSION
These results suggest it is necessary to not only manage symptoms, but also apply interventions to increase social support and cognitive appraisal about sleep in order to increase QOL in patients with obstructive sleep apnea.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Depression/etiology
Hospitals, University
Humans
Male
Middle Aged
*Models, Theoretical
Polysomnography
*Quality of Life
Questionnaires
Severity of Illness Index
Sleep Apnea, Obstructive/complications/*psychology
Sleep Initiation and Maintenance Disorders/etiology
Social Support
Tertiary Care Centers
Young Adult
Figure
Reference
-
1. Akashiba T, Kawahara S, Akahoshi T, Omori C, Saito O, Majima T, et al. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest. 2002. 122(3):861–865. http://dx.doi.org/10.1378/chest.122.3.861.2. American Academy of Sleep Medicine. The international classification of sleep disorders: Diagnostic and coding manual. 2005. 2nd ed. Westchester, IL: Author.3. Bae BR. Structural equation modeling with AMOS 19: Principles and practice. 2011. Seoul: CheongRam Publishing.4. Balsevicius T, Uloza V, Sakalauskas R, Miliauskas S. Peculiarities of clinical profile of snoring and mild to moderate obstructive sleep apnea-hypopnea syndrome patients. Sleep Breath. 2012. 16(3):835–843. http://dx.doi.org/10.1007/s11325-011-0584-z.5. Beck AT, Steer RA, Brown GK. Manual for the BDI-II, the psychological corporation. 1996. San Antonio, TX: Psychological Corporation.6. Bixler EO, Vgontzas AN, Lin HM, Calhoun SL, Vela-Bueno A, Kales A. Excessive daytime sleepiness in a general population sample: The role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab. 2005. 90(8):4510–4515. http://dx.doi.org/10.1210/jc.2005-0035.7. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987. 40(5):373–383. http://dx.doi.org/10.1016/0021-9681(87)90171-8.8. Collop N. The effect of obstructive sleep apnea on chronic medical disorders. Cleve Clin J Med. 2007. 74(1):72–78. http://dx.doi.org/10.3949/ccjm.74.1.72.9. Ferrans CE, Zerwic JJ, Wilbur JE, Larson JL. Conceptual model of health-related quality of life. J Nurs Scholarsh. 2005. 37(4):336–342. http://dx.doi.org/10.1111/j.1547-5069.2005.00058.x.10. Flemons WW, Reimer MA. Development of a disease-specific health-related quality of life questionnaire for sleep apnea. Am J Respir Crit Care Med. 1998. 158(2):494–503.11. Gélinas C, Fillion L. Factors related to persistent fatigue following completion of breast cancer treatment. Oncol Nurs Forum. 2004. 31(2):269–278. http://dx.doi.org/10.1188/04.onf.269-278.12. Jennum P, Kjellberg J. Health, social and economical consequences of sleep-disordered breathing: A controlled national study. Thorax. 2011. 66(7):560–566. http://10.1136/thx.2010.143958.13. Johns MW. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep. 1991. 14(6):540–545.14. Kapur V, Strohl KP, Redline S, Iber C, O'Connor G, Nieto J. Underdiagnosis of sleep apnea syndrome in U.S. communities. Sleep Breath. 2002. 6(2):49–54. http://dx.doi.org/10.1007/s11325-002-0049-5.15. Karademas EC. Self-efficacy, social support and well-being: The mediating role of optimism. Pers Individ Dif. 2006. 40(6):1281–1290.16. Kim J, In K, You S, Kang K, Shim J, Lee S, et al. Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004. 170(10):1108–1113. http://dx.doi.org/10.1164/rccm.200404-519OC.17. Korea Centers for Disease Control and Prevention. The fourth Korea national health and nutrition examination survey [KNHANES IV-2] data. 2010. 01. 01. Retrieved February 15, 2010. from http://knhanes.cdc.go.kr/.18. Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet. 2005. 365(9464):1046–1053. http://dx.doi.org/10.1016/s0140-6736(05)71141-7.19. Morin CM. Insomnia: Psychological assessment and management. 1993. New York: Guilford Press.20. Morin CM, Vallières A, Ivers H. Dysfunctional beliefs and attitudes about sleep (DBAS): Validation of a brief version (DBAS-16). Sleep. 2007. 30(11):1547–1554.21. Pepin JL, Viot-Blanc V, Escourrou P, Racineux JL, Sapene M, Lévy P, et al. Prevalence of residual excessive sleepiness in CPAPtreated sleep apnoea patients: The French multicentre study. Eur Respir J. 2009. 33(5):1062–1067. http://dx.doi.org/10.1183/09031936.00016808.22. Pinto LR Jr, Pinto MC, Goulart LI, Truksinas E, Rossi MV, Morin CM, et al. Sleep perception in insomniacs, sleep-disordered breathing patients, and healthy volunteers--an important biologic parameter of sleep. Sleep Med. 2009. 10(8):865–868. http://dx.doi.org/10.1016/j.sleep.2008.06.016.23. Salaffi F, Carotti M, Gasparini S, Intorcia M, Grassi W. The health-related quality of life in rheumatoidarthritis, ankylosing spondylitis, and psoriatic arthritis: A comparison with a selected sample of healthy people. Health Qual Life Outcomes. 2009. 7:25. http://dx.doi.org/10.1186/1477-7525-7-25.24. Smith S, Sullivan K, Hopkins W, Douglas J. Frequency of insomnia report in patients with obstructive sleep apnoea hypopnea syndrome (OSAHS). Sleep Med. 2004. 5(5):449–456. http://10.1016/j.sleep.2004.03.005.25. Strine TW, Chapman DP, Balluz L, Mokdad AH. Health-related quality of life and health behaviors by social and emotional support. Their relevance to psychiatry and medicine. Soc Psychiatry Psychiatr Epidemiol. 2008. 43(2):151–159. http://dx.doi.org/10.1007/s00127-007-0277-x.26. Vozoris NT, Leung RS. Sedative medication use: Prevalence, risk factors, and associations with body mass index using population-level data. Sleep. 2011. 34(7):869–874. http://dx.doi.org/10.5665/sleep.1116.27. Weaver EM, Woodson BT, Steward DL. Polysomnography indexes are discordant with quality of life, symptoms, and reaction times in sleep apnea patients. Otolaryngol Head Neck Surg. 2005. 132(2):255–262. http://dx.doi.org/10.1016/j.otohns.2004.11.001.28. Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995. 273(1):59–65.29. Ye L, Liang ZA, Weaver TE. Predictors of health-related quality of life in patients with obstructive sleep apnoea. J Adv Nurs. 2008. 63(1):54–63. http://dx.doi.org/10.1111/j.1365-2648.2008.04652.x.30. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988. 52(1):30–41. http://dx.doi.org/10.1207/s15327752jpa5201_2.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Allergic Rhinitis and Sleep-disordered Breathing
- Structural equation modeling for association between patient satisfaction and quality of life after implant surgery
- Pathophysiology and Diagnosis of Sleep Apnea
- Correlation between Quality of Life and Indices of Polysomnography in Children with Obstructive Sleep Apnea Syndrome
- Obstructive Sleep Apnea in Interstitial Lung Disease