Yonsei Med J.
2013 May;54(3):686-689. 10.3349/ymj.2013.54.3.686.
Studies on Therapeutic Effects and Pathological Features of an Antithrombin Preparation in Septic Disseminated Intravascular Coagulation Patients
- Affiliations
-
- 1Department of Emergency and Critical Care Medicine, Saga University Hospital, Saga, Japan. sakamoy@cc.saga-u.ac.jp
- 2Department of Emergency and Critical Care Medicine, Nippon Medical School Chiba Hokusou Hospital, Chiba, Japan.
- 3Department of Emergency Medicine, Nippon Medical School, Tokyo, Japan.
- KMID: 1727883
- DOI: http://doi.org/10.3349/ymj.2013.54.3.686
Abstract
- PURPOSE
Few reports have been made on the therapeutic effects as well as pathological features of an antithrombin preparation in patients diagnosed with septic disseminated intravascular coagulation (DIC) by the diagnostic criteria for acute DIC.
MATERIALS AND METHODS
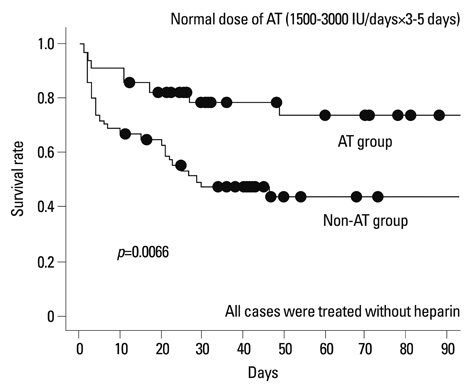
A total of 88 sepsis patients who had received inpatient hospital care during the period from January 2000 through December 2008 were divided into two groups, an antithrombin group and a non-antithrombin group, to study the outcomes. Furthermore, the relationship between sepsis-related factors and DIC in 44 patients was studied.
RESULTS
The antithrombin group contained 34 patients, and the non-antithrombin group contained 54 patients. The outcomes were significantly better in the antithrombin group. The levels of protein C were low in DIC patients.
CONCLUSION
Our results suggest that early administration of antithrombin might improve outcomes of septic DIC patients in the diagnostic criteria for Japanese Association for Acute Medicine acute DIC.
Keyword
MeSH Terms
Figure
Reference
-
1. Kushimoto S, Gando S, Saitoh D, Ogura H, Mayumi T, Koseki K, et al. Clinical course and outcome of disseminated intravascular coagulation diagnosed by Japanese Association for Acute Medicine criteria. Comparison between sepsis and trauma. Thromb Haemost. 2008. 100:1099–1105.
Article2. Petros S, Kliem P, Siegemund T, Siegemund R. Thrombin generation in severe sepsis. Thromb Res. 2012. 129:797–800.
Article3. Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004. 32:858–873.
Article4. Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008. 36:296–327.
Article5. Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001. 344:699–709.
Article6. Ranieri VM, Thompson BT, Barie PS, Dhainaut JF, Douglas IS, Finfer S, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012. 366:2055–2064.
Article7. Gando S, Iba T, Eguchi Y, Ohtomo Y, Okamoto K, Koseki K, et al. A multicenter, prospective validation of disseminated intravascular coagulation diagnostic criteria for critically ill patients: comparing current criteria. Crit Care Med. 2006. 34:625–631.
Article8. Wagner DP, Draper EA. Acute physiology and chronic health evaluation (APACHE II) and Medicare reimbursement. Health Care Financ Rev. 1984. Suppl. 91–105.9. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996. 22:707–710.
Article10. Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M. Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH). Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001. 86:1327–1330.
Article11. Wada H, Sase T, Matsumoto T, Kushiya F, Sakakura M, Mori Y, et al. Increased soluble fibrin in plasma of patients with disseminated intravascular coagulation. Clin Appl Thromb Hemost. 2003. 9:233–240.
Article12. Silva E, de Figueiredo LF, Colombari F. Prowess-shock trial: a protocol overview and perspectives. Shock. 2010. 34:Suppl 1. 48–53.13. Eisele B, Lamy M, Thijs LG, Keinecke HO, Schuster HP, Matthias FR, et al. Antithrombin III in patients with severe sepsis. A randomized, placebo-controlled, double-blind multicenter trial plus a meta-analysis on all randomized, placebo-controlled, double-blind trials with antithrombin III in severe sepsis. Intensive Care Med. 1998. 24:663–672.14. Baudo F, Caimi TM, de Cataldo F, Ravizza A, Arlati S, Casella G, et al. Antithrombin III (ATIII) replacement therapy in patients with sepsis and/or postsurgical complications: a controlled double-blind, randomized, multicenter study. Intensive Care Med. 1998. 24:336–342.
Article15. Wiedermann CJ, Kaneider NC. A systematic review of antithrombin concentrate use in patients with disseminated intravascular coagulation of severe sepsis. Blood Coagul Fibrinolysis. 2006. 17:521–526.
Article16. Welcker K, Lederle J, Schorr M, Siebeck M. Surgery and adjuvant therapy in patients with diffuse peritonitis: cost analysis. World J Surg. 2002. 26:307–313.17. Kienast J, Juers M, Wiedermann CJ, Hoffmann JN, Ostermann H, Strauss R, et al. Treatment effects of high-dose antithrombin without concomitant heparin in patients with severe sepsis with or without disseminated intravascular coagulation. J Thromb Haemost. 2006. 4:90–97.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antithrombin III in the Diagnosis and Treatment of Disseminated Intravascular Coagulation in Premature Infants
- Erratum: Current Pathological and Laboratory Considerations in the Diagnosis of Disseminated Intravascular Coagulation
- The Effects of Antithrombin III on Disseminated Intravascular Coagulation(DIC) in Premature Infants
- Disseminated Intravascular Coagulation Following Septic Shock in Multiple Open Fractures : a Case Report
- A Case of Septic Shock and Disseminated Intravascular Coagulation Complicated by Acute Myocardial Infarction Following Amniocentesis