Clin Orthop Surg.
2010 Dec;2(4):227-231. 10.4055/cios.2010.2.4.227.
Treatment of Subtrochanteric Femoral Fractures Using Selfdynamisable Internal Fixator
- Affiliations
-
- 1Clinic for Orthopedic Surgery and Traumatology, Faculty of Medicine, Clinical Center, Nis, Serbia.
- 2Department of Orthopaedic Surgery, Kyungpook National University Hospital, Daegu, Korea.
- 3Department of Orthopaedic Surgery, Asan Medical Center, Seoul, Korea. jeonchoi@chol.com
- KMID: 1719323
- DOI: http://doi.org/10.4055/cios.2010.2.4.227
Abstract
- BACKGROUND
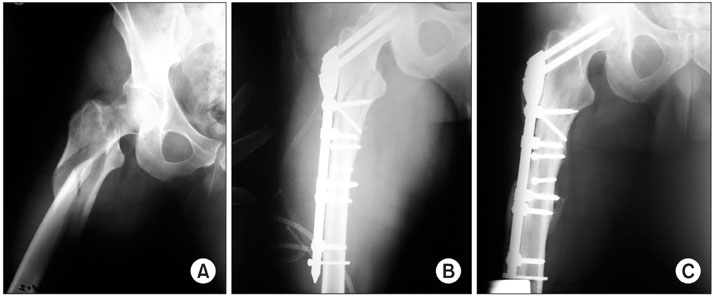
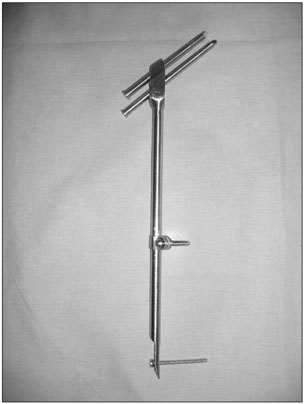
Surgical treatment is the preferred method for treating subtrochanteric femoral fractures and the variety of extramedullary and intramedullary implants continues to evolve. The purpose of our study was to retrospectively evaluate the clinical and radiological results of subtrochanteric fractures that are treated with the Selfdynamisable internal fixator.
METHODS
From January 2000 to January 2004, we treated 49 consecutive patients who had subtrochanteric fractures. According to the AO classification, 8 (16.3%) fractures were type 32-A, 16 (32.7%) were type 32-B and 25 (51%) fractures were type 32-C. The mean follow-up time was 22.3 months.
RESULTS
The average operating time was 45 minutes (range, 32 to 90 minutes). The average blood loss was 250 mL (range, 125 to 350 mL). The average hospital stay was 10 days (range, 7 to 59 days). Implant failure was not observed and union was achieved in all the patients. Deep infection occurred in one (2%) patient in the early postoperative period. Fracture union was achieved at a mean of 14 weeks. Varus malalignment less then 10 degree was noted in three (6.1%) patients at the end of follow-up. Thirty-five patients were pain-free and 14 had mild pain.
CONCLUSIONS
The selfdynamisable internal fixator was successfully used for subtrochanteric fracture. It provides a short operative time, low blood loss, spontaneous biaxial dynamisation and healing in an optimal period of time without the need for secondary intervention.
MeSH Terms
Figure
Cited by 1 articles
-
The Treatment of Subtrochanteric Fractures with Proximal Femoral Nail Antirotation
Chi Hyoung Pak, Sang Hong Lee, Sang Ho Ha, Gwang Chul Lee, Kyoung Chul Song
J Korean Fract Soc. 2013;26(4):284-291. doi: 10.12671/jkfs.2013.26.4.284.
Reference
-
1. Robinson CM, Court-Brown CM, McQueen MM, Christie J. Hip fractures in adults younger than 50 years of age. Epidemiology and results. Clin Orthop Relat Res. 1995. (312):238–246.2. Koval KJ, Egol KA, Zuckerman JD. Dee R, Hurst LC, Gruber MA, Kottmeier SA, editors. Hip fractures and dislocations. Principles of orthopaedic practice. 1997. 2nd ed. NewYork: McGraw-Hill;465–481.3. Datir SP, Bedi GS, Curwen CH. Unreamed femoral nail with spiral blade in subtrochanteric fractures: experience of 55 cases. Injury. 2004. 35(2):191–195.
Article4. Borens O, Wettstein M, Kombot C, Chevalley F, Mouhsine E, Garofalo R. Long gamma nail in the treatment of subtrochanteric fractures. Arch Orthop Trauma Surg. 2004. 124(7):443–447.
Article5. Hotz TK, Zellweger R, Kach KP. Minimal invasive treatment of proximal femur fractures with the long gamma nail: indication, technique, results. J Trauma. 1999. 47(5):942–945.
Article6. Roberts CS, Nawab A, Wang M, Voor MJ, Seligson D. Second generation intramedullary nailing of subtrochanteric femur fractures: a biomechanical study of fracture site motion. J Orthop Trauma. 2002. 16(4):231–238.
Article7. Blatter G, Janssen M. Treatment of subtrochanteric fractures of the femur: reduction on the traction table and fixation with dynamic condylar screw. Arch Orthop Trauma Surg. 1994. 113(3):138–141.
Article8. Brien WW, Wiss DA, Becker V Jr, Lehman T. Subtrochanteric femur fractures: a comparison of the Zickel nail, 95 degrees blade plate, and interlocking nail. J Orthop Trauma. 1991. 5(4):458–464.9. Vaidya SV, Dholakia DB, Chatterjee A. The use of a dynamic condylar screw and biological reduction techniques for subtrochanteric femur fracture. Injury. 2003. 34(2):123–128.
Article10. Kulkarni SS, Moran CG. Results of dynamic condylar screw for subtrochanteric fractures. Injury. 2003. 34(2):117–122.
Article11. Mitkovic M, Bumbasirevic M, Golubovic Z, et al. New biological method of internal fixation of the femur. Acta Chir Iugosl. 2005. 52(2):113–116.
Article12. Muller ME, Nazarian S, Koch P. The AO classification of fractures. 1988. New York: Springer.13. Tornetta P 3rd. Subtrochanteric femur fracture. J Orthop Trauma. 2002. 16(4):280–283.
Article14. Grosse A, Favreul E, Taglang G. The long gamma nail experience: 79 cases. Orthopedics. 1994. 2(1):3–5.15. Hoover GK, Browner BD, Cole JD, Comstock CP, Cotler HB. Initial experience with a second generation locking femoral nail: the Russell-Taylor reconstruction nail. Contemp Orthop. 1991. 23(3):199–208.16. Cheng MT, Chiu FY, Chuang TY, Chen CM, Chen TH, Lee PC. Treatment of complex subtrochanteric fracture with the long gamma AP locking nail: a prospective evaluation of 64 cases. J Trauma. 2005. 58(2):304–311.17. Miedel R, Ponzer S, Tornkvist H, Soderqvist A, Tidermark J. The standard Gamma nail or the Medoff sliding plate for unstable trochanteric and subtrochanteric fractures: a randomised, controlled trial. J Bone Joint Surg Br. 2005. 87(1):68–75.18. Kinast C, Bolhofner BR, Mast JW, Ganz R. Subtrochanteric fractures of the femur: results of treatment with the 95 degrees condylar blade-plate. Clin Orthop Relat Res. 1989. (238):122–130.19. Nungu KS, Olerud C, Rehnberg L. Treatment of subtrochanteric fractures with the AO dynamic condylar screw. Injury. 1993. 24(2):90–92.
Article20. Ruff ME, Lubbers LM. Treatment of subtrochanteric fractures with a sliding screw-plate device. J Trauma. 1986. 26(1):75–80.
Article21. Sanders R, Regazzoni P. Treatment of subtrochanteric femur fractures using the dynamic condylar screw. J Orthop Trauma. 1989. 3(3):206–213.
Article22. Siebenrock KA, Muller U, Ganz R. Indirect reduction with a condylar blade plate for osteosynthesis of subtrochanteric femoral fractures. Injury. 1998. 29:Suppl 3. C7–C15.
Article23. Lunsjo K, Ceder L, Thorngren KG, et al. Extramedullary fixation of 569 unstable intertrochanteric fractures: a randomized multicenter trial of the Medoff sliding plate versus three other screw-plate systems. Acta Orthop Scand. 2001. 72(2):133–140.
Article24. Goldhagen PR, O'Connor DR, Schwarze D, Schwartz E. A prospective comparative study of the compression hip screw and the gamma nail. J Orthop Trauma. 1994. 8(5):367–372.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Subtrochanteric Fracture of Femur with Spiral Blade Unreamed Intramedullary Femoral Nail
- Subtrochanteric Fracture after Cannulatd Screw Fixation of Femoral Neck Fracture in a Child: A Case Report
- Surgical Treatment of the Atypical Femoral Fracture: Overcoming Femoral Bowing
- Subtrochanteric Fracture: Emphasis on Surgical Techniques in Nailing
- Epidemiology and Clinical Features of Atypical Femoral Fractures