Clin Orthop Surg.
2010 Dec;2(4):203-208. 10.4055/cios.2010.2.4.203.
Revision Surgery after Vertebroplasty or Kyphoplasty
- Affiliations
-
- 1Department of Orthopaedic Surgery, The Catholic University of Korea School of Medicine, Seoul, Korea. boscoa@empal.com
- KMID: 1719319
- DOI: http://doi.org/10.4055/cios.2010.2.4.203
Abstract
- BACKGROUND
We wanted to investigate the leading cause of failed vertebroplasty or kyphoplasty.
METHODS
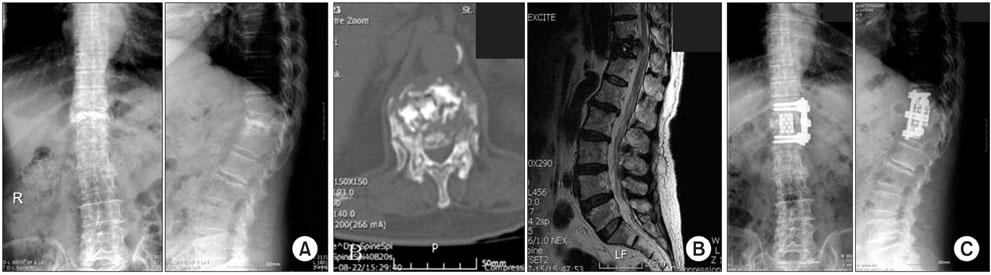
Twelve patients (10 females and 2 males) who underwent revision surgery after vertebroplasty or kyphoplasty were included. In 4 cases, vertebroplasty was done for two or more levels. Six cases with kyphoplasty were included. Through the retrospective review of the radiographic studies and medical record, we analyzed the etiology of the revision surgery.
RESULTS
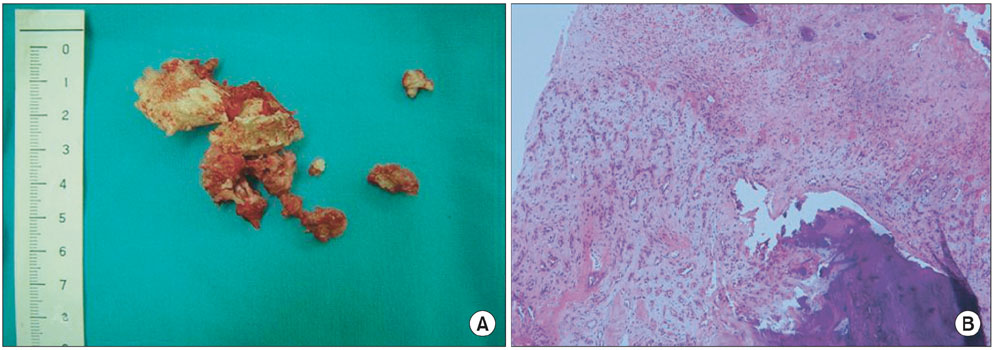
Uncontrolled back pain was the main clinical presentation. In 4 cases, neurological symptoms were noted, including one case with conus medullaris syndrome. The average time to the revision surgery after vertebroplasty or kyphoplasty was 15 months. Infection (4 cases) and progressive kyphosis with collapse (8 cases) were the causes for the revision. A solid pattern of inserted bone cement and bone resorption around the cement were noted in the all cases with progressive collapse and kyphosis.
CONCLUSIONS
Infection, misdiagnosis and progressive kyphosis were causes of the revision surgery after vertebroplasty and kyphoplasty. A solid pattern of accumulation of bone cement and peri-cement bone resorption might be related with the progressive collapse.
MeSH Terms
Figure
Cited by 1 articles
-
Bone Cement Dislodgement: One of Complications Following Bone Cement Augmentation Procedures for Osteoporotic Spinal Fracture
Kee-Yong Ha, Young-Hoon Kim, Sung-Rim Yoo, Jan Noel Molon
J Korean Neurosurg Soc. 2015;57(5):367-370. doi: 10.3340/jkns.2015.57.5.367.
Reference
-
1. Galibert P, Deramond H, Rosat P, Le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987. 33(2):166–168.2. Fribourg D, Tang C, Sra P, Delamarter R, Bae H. Incidence of subsequent vertebral fracture after kyphoplasty. Spine (Phila Pa 1976). 2004. 29(20):2270–2276.
Article3. Lin EP, Ekholm S, Hiwatashi A, Westesson PL. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004. 25(2):175–180.4. Alfonso Olmos M, Silva Gonzalez A, Duart Clemente J, Villas Tome C. Infected vertebroplasty due to uncommon bacteria solved surgically: a rare and threatening life complication of a common procedure: report of a case and a review of the literature. Spine (Phila Pa 1976). 2006. 31(20):E770–E773.5. Quesada N, Mutlu GM. Images in cardiovascular medicine: pulmonary embolization of acrylic cement during vertebroplasty. Circulation. 2006. 113(8):e295–e296.6. Shin KS, Kim JS, Lee DW, Kim JS, Heo JK. Surgical treatment of root injury after percutaneous vertebroplasty: case report. J Korean Soc Spine Surg. 2002. 9(1):54–58.
Article7. Trout AT, Kallmes DF, Lane JI, Layton KF, Marx WF. Subsequent vertebral fractures after vertebroplasty: association with intraosseous clefts. AJNR Am J Neuroradiol. 2006. 27(7):1586–1591.8. Uppin AA, Hirsch JA, Centenera LV, Pfiefer BA, Pazianos AG, Choi IS. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 2003. 226(1):119–124.
Article9. Lane JI, Maus TP, Wald JT, Thielen KR, Bobra S, Luetmer PH. Intravertebral clefts opacified during vertebroplasty: pathogenesis, technical implications, and prognostic significance. AJNR Am J Neuroradiol. 2002. 23(10):1642–1646.10. Melton LJ 3rd, Chrischilles EA, Cooper C, Lane AW, Riggs BL. Perspective: how many women have osteoporosis? J Bone Miner Res. 1992. 7(9):1005–1010.
Article11. Deramond H, Depriester C, Galibert P, Le Gars D. Percutaneous vertebroplasty with polymethylmethacrylate: technique, indications, and results. Radiol Clin North Am. 1998. 36(3):533–546.12. Won JH, Yeom JS, Park SK, Lee JH, Chang BS, Lee CK. Two simple tests for adequate needle positioning in vertebroplasty. J Korean Soc Spine Surg. 2006. 13(2):101–105.
Article13. Lindsay R, Silverman SL, Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001. 285(3):320–323.
Article14. Schmid KE, Boszczyk BM, Bierschneider M, Zarfl A, Robert B, Jaksche H. Spondylitis following vertebroplasty: a case report. Eur Spine J. 2005. 14(9):895–899.
Article15. Vats HS, McKiernan FE. Infected vertebroplasty: case report and review of literature. Spine (Phila Pa 1976). 2006. 31(22):E859–E862.16. Yu SW, Chen WJ, Lin WC, Chen YJ, Tu YK. Serious pyogenic spondylitis following vertebroplasty: a case report. Spine (Phila Pa 1976). 2004. 29(10):E209–E211.17. Grados F, Depriester C, Cayrolle G, Hardy N, Deramond H, Fardellone P. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford). 2000. 39(12):1410–1414.
Article18. Belkoff SM, Mathis JM, Fenton DC, Scribner RM, Reiley ME, Talmadge K. An ex vivo biomechanical evaluation of an inflatable bone tamp used in the treatment of compression fracture. Spine (Phila Pa 1976). 2001. 26(2):151–156.
Article19. Berlemann U, Ferguson SJ, Nolte LP, Heini PF. Adjacent vertebral failure after vertebroplasty: a biomechanical investigation. J Bone Joint Surg Br. 2002. 84(5):748–752.20. Oka M, Matsusako M, Kobayashi N, Uemura A, Numaguchi Y. Intravertebral cleft sign on fat-suppressed contrast-enhanced MR: correlation with cement distribution pattern on percutaneous vertebroplasty. Acad Radiol. 2005. 12(8):992–999.21. Ha KY, Lee JS, Kim KW, Chon JS. Percutaneous vertebroplasty for vertebral compression fractures with and without intravertebral clefts. J Bone Joint Surg Br. 2006. 88(5):629–633.
Article22. Togawa D, Bauer TW, Lieberman IH, Takikawa S. Histologic evaluation of human vertebral bodies after vertebral augmentation with polymethyl methacrylate. Spine (Phila Pa 1976). 2003. 28(14):1521–1527.
Article23. Togawa D, Kovacic JJ, Bauer TW, Reinhardt MK, Brodke DS, Lieberman IH. Radiographic and histologic findings of vertebral augmentation using polymethylmethacrylate in the primate spine: percutaneous vertebroplasty versus kyphoplasty. Spine (Phila Pa 1976). 2006. 31(1):E4–E10.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Commentary on “Utilization of Vertebroplasty/Kyphoplasty in the Management of Compression Fractures: National Trends and Predictors of Vertebroplasty/Kyphoplasty”
- Comparisons of Vertebroplasty and Kyphoplasty for Thoracolumbar Osteoporotic Vertebral Fractures
- Minimally Invasive Treatment of Painful Osteoporotic Vertebral Fractures
- Utilization of Vertebroplasty/Kyphoplasty in the Management of Compression Fractures: National Trends and Predictors of Vertebroplasty/Kyphoplasty
- The Incidence of Recurrent Vertebral Fracture after Kyphoplasty or Vertebroplasty