Yonsei Med J.
2006 Jun;47(3):319-325. 10.3349/ymj.2006.47.3.319.
Posterior Lumbar Interbody Fusion via a Unilateral Approach
- Affiliations
-
- 1Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea. knkim@yumc.yonsei.ac.kr
- KMID: 1715849
- DOI: http://doi.org/10.3349/ymj.2006.47.3.319
Abstract
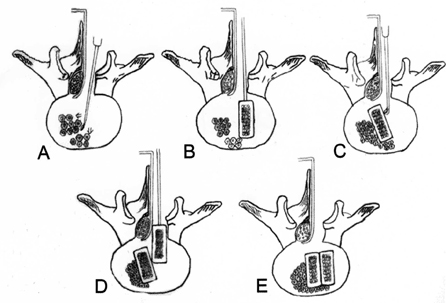
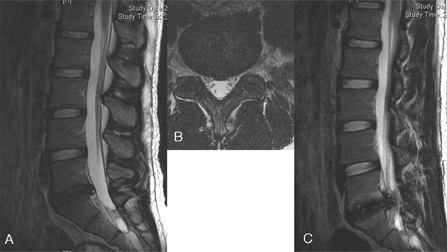
- This study sought to determine the outcomes of posterior lumbar interbody fusion (PLIF), via a unilateral approach, in selected patients who presented with unilateral leg pain and segmental instability of the lumbar spine. Patients with a single level of a herniated disc disease in the lumbar spine, unilateral leg pain, chronic disabling lower back pain (LBP), and a failed conservative treatment, were considered for the procedure. A total of 41 patients underwent a single-level PLIF using two PEEK(TM) (Poly-Ether-Ether-Ketone) cages filled with iliac bone, via a unilateral approach. The patients comprised 21 women and 20 men with a mean age of 41 years (range: 22 to 63 years). Two cages were inserted using a unilateral medial facetectomy and a partial hemilaminectomy. At follow-up, the outcomes were assessed using the Prolo Scale. The success of the fusion was determined by dynamic lumbar radiography and/or computerized tomography scanning. All the patients safely underwent surgery without severe complications. During a mean follow-up period of 26 months, 1 patient underwent percutaneous pedicle screw fixation due to persistent LBP. A posterior displacement of the cage was found in one patient. At the last follow up, 90% of the patients demonstrated satisfactory results. An osseous fusion was present in 85% of the patients. A PLIF, via a unilateral approach, enables a solid union with satisfactory clinical results. This preserves part of the posterior elements of the lumbar spine in selected patients with single level instability and unilateral leg pain.
MeSH Terms
Figure
Cited by 2 articles
-
Cantilever Transforaminal Lumbar Interbody Fusion for Upper Lumbar Degenerative Diseases (Minimum 2 Years Follow Up)
Akira Hioki, Kei Miyamoto, Hideo Hosoe, Seiichi Sugiyama, Naoki Suzuki, Katsuji Shimizu
Yonsei Med J. 2011;52(2):314-321. doi: 10.3349/ymj.2011.52.2.314.Posterior Lumbar Interbody Fusion Using a Unilateral Single Cage and a Local Morselized Bone Graft in the Degenerative Lumbar Spine
Dong-Hee Kim, Soon-Taek Jeong, Sang-Soo Lee
Clin Orthop Surg. 2009;1(4):214-221. doi: 10.4055/cios.2009.1.4.214.
Reference
-
1. Axelsson P, Johnsson R, Stromqvist B, Arvidsson M, Herrlin K. Posterolateral lumbar fusion. Outcome of 71 consecutive operations after 4 (2-7) years. Acta Orthop Scand. 1994. 65:309–314.2. Fritzell P, Hagg O, Wessberg P, Nordwall A. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine. 2002. 27:1131–1141.3. Brislin B, Vaccaro AR. Advances in posterior lumbar interbody fusion. Orthop Clin North Am. 2002. 33:367–374.4. Lin PM, Cautilli RA, Joyce MF. Posterior lumbar interbody fusion. Clin Orthop Relat Res. 1983. 180:154–168.5. Lin PM. Posterior lumbar interbody fusion (PLIF): past, present, and future. Clin Neurosurg. 2000. 47:470–482.6. Hacker RJ. Comparison of interbody fusion approaches for disabling low back pain. Spine. 1997. 22:660–665. discussion 665-6.7. Agazzi S, Reverdin A, May D. Posterior lumbar interbody fusion with cages: an independent review of 71 cases. J Neurosurg. 1999. 91(2):Suppl. 186–192.8. Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine. 1997. 22:210–219. discussion 219-20.9. Brantigan JW, Steffee AD, Geiger JM. A carbon fiber implant to aid interbody lumbar fusion. Mechanical testing. Spine. 1991. 16(6):Suppl. S277–S282.10. Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: preliminary clinical results. J Neurosurg. 2002. 97(1):Suppl. 7–12.11. Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993. 18:575–581.12. Lowe TG, Tahernia AD. Unilateral transforaminal posterior lumbar interbody fusion. Clin Orthop Relat Res. 2002. 394:64–72.13. Moskowitz A. Transforaminal lumbar interbody fusion. Orthop Clin North Am. 2002. 33:359–366.14. Blume HG. Unilateral posterior lumbar interbody fusion: simplified dowel technique. Clin Orthop Relat Res. 1985. 193:75–84.15. Zhao J, Hai Y, Ordway NR, Park CK, Yuan HA. Posterior lumbar interbody fusion using posterolateral placement of a single cylindrical threaded cage. Spine. 2000. 25:425–430.16. Zhao J, Wang X, Hou T, He S. One versus two BAK fusion cages in posterior lumbar interbody fusion to L4-L5 degenerative spondylolisthesis: a randomized, controlled prospective study in 25 patients with minimum two-year follow-up. Spine. 2002. 27:2753–2757.17. Abumi K, Panjabi MM, Kramer KM, Duranceau J, Oxland T, Crisco JJ. Biomechanical evaluation of lumbar spinal stability after graded facetectomies. Spine. 1990. 15:1142–1147.18. Chitnavis B, Barbagallo G, Selway R, Dardis R, Hussain A, Gullan R. Posterior lumbar interbody fusion for revision disc surgery: review of 50 cases in which carbon fiber cages were implanted. J Neurosurg. 2001. 95(2):Suppl. 190–195.19. Turner JA, Ersek M, Herron L, Haselkorn J, Kent D, Ciol MA, et al. Patient outcomes after lumbar spinal fusions. JAMA. 1992. 268:907–911.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mini-invasive unilateral transforaminal lumbar interbody fusion and pedicle screw fixation
- Oblique Posterior Interbody Fusion with Bone Plugs by Unilateral Approach for Treatment of Lumbar Instability: Technical Note
- Evaluation of Posterior Lumbar Interbody Fusion
- Comparison of Unilateral and Bilateral Approaches for Posterior Lumbar Interbody Fusion
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications