Factors Related to Prehospital Time Delay in Acute ST-Segment Elevation Myocardial Infarction
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 2Department of Emergency Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea. ydkim@mail.donga.ac.kr
- KMID: 1714196
- DOI: http://doi.org/10.3346/jkms.2012.27.8.864
Abstract
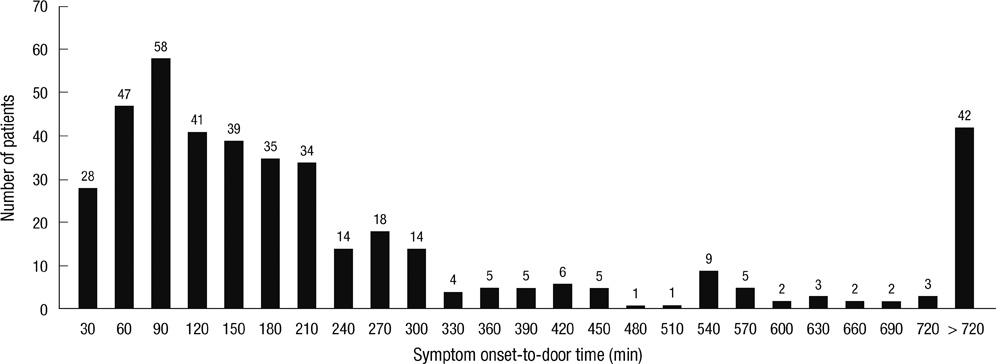
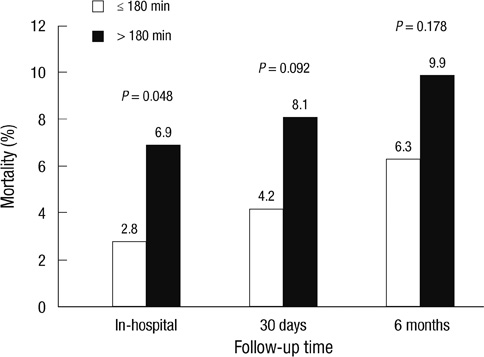
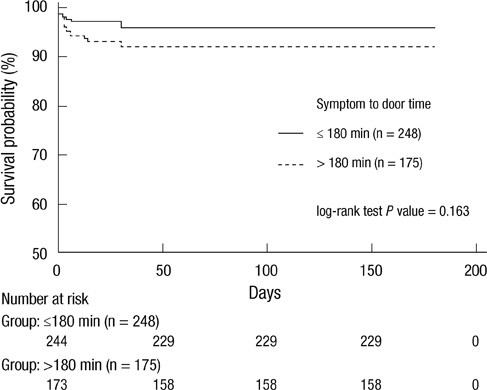
- Despite recent successful efforts to shorten the door-to-balloon time in patients with acute ST-segment elevation myocardial infarction (STEMI), prehospital delay remains unaffected. Nonetheless, the factors associated with prehospital delay have not been clearly identified in Korea. We retrospectively evaluated 423 patients with STEMI. The mean symptom onset-to-door time was 255 +/- 285 (median: 150) min. The patients were analyzed in two groups according to symptom onset-to-door time (short delay group: < or = 180 min vs long delay group: > 180 min). Inhospital mortality was significantly higher in long delay group (6.9% vs 2.8%; P = 0.048). Among sociodemographic and clinical variables, diabetes, low educational level, triage via other hospital, use of private transport and night time onset were more prevalent in long delay group (21% vs 30%; P = 0.038, 47% vs 59%; P = 0.013, 72% vs 82%; P = 0.027, 25% vs 41%; P < 0.001 and 33% vs 48%; P = 0.002, respectively). In multivariate analysis, low educational level (1.66 [1.08-2.56]; P = 0.021), symptom onset during night time (1.97 [1.27-3.04]; P = 0.002), triage via other hospital (1.83 [1.58-5.10]; P = 0.001) and private transport were significantly associated with prehospital delay (3.02 [1.81-5.06]; P < 0.001). In conclusion, prehospital delay is more frequent in patients with low educational level, symptom onset during night time, triage via other hospitals, and private transport, and is associated with higher inhospital mortality.
Keyword
MeSH Terms
Figure
Cited by 6 articles
-
A Simple Protocol to Save Time Delay for Patients with ST-Elevation Myocardial Infarction by Using Pre-hospital Electrocardiogram Transmission Program
Jung-Joon Cha, Soon Jun Hong
Korean Circ J. 2020;50(8):720-722. doi: 10.4070/kcj.2020.0218.Community-Based Pre-Hospital Electrocardiogram Transmission Program for Reducing Systemic Time Delay in Acute ST-Segment Elevation Myocardial Infarction
Kyungil Park, Jong-Sung Park, Young-Rak Cho, Tae-Ho Park, Moo-Hyun Kim, Tae-Hyun Yang, Doo-Il Kim, Jung-Hwan Kim, Yong-Hwan Lee, Dong-Won Lee, Jeongkee Seo, Geun-Young Lee, Young-Dae Kim
Korean Circ J. 2020;50(8):709-719. doi: 10.4070/kcj.2019.0337.Gender Differences in Factors Related to Prehospital Delay in Patients with ST-Segment Elevation Myocardial Infarction
Hee-Sook Kim, Kun-Sei Lee, Sang Jun Eun, Si-Wan Choi, Dae Hyeok Kim, Tae-Ho Park, Kyeong Ho Yun, Dong Heon Yang, Seok Jae Hwang, Ki-Soo Park, Rock Bum Kim
Yonsei Med J. 2017;58(4):710-719. doi: 10.3349/ymj.2017.58.4.710.The Impacts of Living Alone in in-Hospital and One-Year Clinical Outcomes after Acute Myocardial Infarction in Korean Patients
Joon Ho Ahn, Hyun Kuk Kim, Jong Yoon Kim, Jumin Won, Hyeong Won Seo, Young Joon Hong, Ju Han Kim, Myung Ho Jeong, Jeong Gwan Cho, Jong Chun Park, Sook Hee Cho, Youngkeun Ahn
J Lipid Atheroscler. 2015;4(2):115-121. doi: 10.12997/jla.2015.4.2.115.Factors Related to Pre-hospital Delay in Korean Patients with ST-segment Elevation Myocardial Infarction: A Data from the Province of Jeonbuk Regional Cardiovascular Center
Mi Rim Lee, Kyeong Ho Yun, Dong Hyun Kim, Sangwoo Kang, Young Jun Kim, Sun Ho Woo, Young Hoon Jeong, Yong Cheol Kim, Young-Hoon Lee, Jeong Mi Lee, Jum Suk Ko, Sang Jae Rhee, Nam-Ho Kim, Seok Kyu Oh
J Lipid Atheroscler. 2016;5(1):21-26. doi: 10.12997/jla.2016.5.1.21.Identifying and Solving Gaps in Pre- and In-Hospital Acute Myocardial Infarction Care in Asia-Pacific Countries
Paul Jie Wen Tern, Amar Vaswani, Khung Keong Yeo
Korean Circ J. 2023;53(9):594-605. doi: 10.4070/kcj.2023.0169.
Reference
-
1. Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009. 119:e21–e181.2. Hong JS, Kang HC, Lee SH, Kim J. Long-term trend in the incidence of acute myocardial infarction in Korea: 1997-2007. Korean Circ J. 2009. 39:467–476.3. De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004. 109:1223–1225.4. Kloner RA, Jennings RB. Consequences of brief ischemia: stunning, preconditioning, and their clinical implications: part 1. Circulation. 2001. 104:2981–2989.5. Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008. 29:2909–2945.6. Schomig A, Ndrepepa G, Mehilli J, Schwaiger M, Schuhlen H, Nekolla S, Pache J, Martinoff S, Bollwein H, Kastrati A. Therapy-dependent influence of time-to-treatment interval on myocardial salvage in patients with acute myocardial infarction treated with coronary artery stenting or thrombolysis. Circulation. 2003. 108:1084–1088.7. Francone M, Bucciarelli-Ducci C, Carbone I, Canali E, Scardala R, Calabrese FA, Sardella G, Mancone M, Catalano C, Fedele F, et al. Impact of primary coronary angioplasty delay on myocardial salvage, infarct size, and microvascular damage in patients with ST-segment elevation myocardial infarction: insight from cardiovascular magnetic resonance. J Am Coll Cardiol. 2009. 54:2145–2153.8. Gersh BJ, Anderson JL. Thrombolysis and myocardial salvage. Results of clinical trials and the animal paradigm: paradoxic or predictable? Circulation. 1993. 88:296–306.9. Nam YH, Cha KS, Kim JH, Park SY, Park TH, Kim MH, Kim YD. Reduction of door-to-balloon time by new performance processes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Angiology. 2011. 62:257–264.10. Blankenship JC, Scott TD, Skelding KA, Haldis TA, Tompkins-Weber K, Sledgen MY, Donegan MA, Buckley JW, Sartorius JA, Hodgson JM, et al. Door-to-balloon times under 90 min can be routinely achieved for patients transferred for ST-segment elevation myocardial infarction percutaneous coronary intervention in a rural setting. J Am Coll Cardiol. 2011. 57:272–279.11. Gross BW, Dauterman KW, Moran MG, Kotler TS, Schnugg SJ, Rostykus PS, Ross AM, Weaver WD. An approach to shorten time to infarct artery patency in patients with ST-segment elevation myocardial infarction. Am J Cardiol. 2007. 99:1360–1363.12. McGinn AP, Rosamond WD, Goff DC Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987-2000. Am Heart J. 2005. 150:392–400.13. Goldberg RJ, Gurwitz JH, Gore JM. Duration of, and temporal trends (1994-1997) in, prehospital delay in patients with acute myocardial infarction: the second National Registry of Myocardial Infarction. Arch Intern Med. 1999. 159:2141–2147.14. Turi ZG, Stone PH, Muller JE, Parker C, Rude RE, Raabe DE, Jaffe AS, Hartwell TD, Robertson TL, Braunwald E. Implications for acute intervention related to time of hospital arrival in acute myocardial infarction. Am J Cardiol. 1986. 58:203–209.15. Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. Eur Heart J. 2007. 28:2525–2538.16. Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation. 2004. 110:e82–e292.17. Kim JA, Jeong JO, Ahn KT, Park HS, Jang WI, Kim MS, Kim JH, Park JH, Lee JH, Choi SW, et al. Causative factors for time delays in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Korean J Med. 2010. 78:586–594.18. Song YB, Hahn JY, Gwon HC, Kim JH, Lee SH, Jeong MH. The impact of initial treatment delay using primary angioplasty on mortality among patients with acute myocardial infarction: from the Korea acute myocardial infarction registry. J Korean Med Sci. 2008. 23:357–364.19. Nguyen HL, Gore JM, Saczynski JS, Yarzebski J, Reed G, Spencer FA, Goldberg RJ. Age and sex differences and 20-year trends (1986 to 2005) in prehospital delay in patients hospitalized with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010. 3:590–598.20. Perkins-Porras L, Whitehead DL, Strike PC, Steptoe A. Pre-hospital delay in patients with acute coronary syndrome: factors associated with patient decision time and home-to-hospital delay. Eur J Cardiovasc Nurs. 2009. 8:26–33.21. Saczynski JS, Yarzebski J, Lessard D, Spencer FA, Gurwitz JH, Gore JM, Goldberg RJ. Trends in prehospital delay in patients with acute myocardial infarction (from the Worcester Heart Attack Study). Am J Cardiol. 2008. 102:1589–1594.22. Berton G, Cordiano R, Palmieri R, Guarnieri G, Stefani M, Palatini P. Clinical features associated with pre-hospital time delay in acute myocardial infarction. Ital Heart J. 2001. 2:766–771.23. Sheifer SE, Rathore SS, Gersh BJ, Weinfurt KP, Oetgen WJ, Breall JA, Schulman KA. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation. 2000. 102:1651–1656.24. Dracup K, McKinley SM, Moser DK. Australian patients' delay in response to heart attack symptoms. Med J Aust. 1997. 166:233–236.25. Foraker RE, Rose KM, McGinn AP, Suchindran CM, Goff DC Jr, Whitsel EA, Wood JL, Rosamond WD. Neighborhood income, health insurance, and prehospital delay for myocardial infarction: the atherosclerosis risk in communities study. Arch Intern Med. 2008. 168:1874–1879.26. Ribeiro S, Gaspar A, Rocha S, Nabais S, Azevedo P, Salgado A, Pereira MA, Correia A. Predictors of pre-hospital delay in patients with ST-segment elevation myocardial infarction. Rev Port Cardiol. 2010. 29:1521–1532.27. Postma S, Dambrink JH, de Boer MJ, Gosselink AT, Eggink GJ, van de Wetering H, Hollak F, Ottervanger JP, Hoorntje JC, Kolkman E, et al. Prehospital triage in the ambulance reduces infarct size and improves clinical outcome. Am Heart J. 2011. 161:276–282.28. Zijlstra F, Patel A, Jones M, Grines CL, Ellis S, Garcia E, Grinfeld L, Gibbons RJ, Ribeiro EE, Ribichini F, et al. Clinical characteristics and outcome of patients with early (<2 h), intermediate (2-4 h) and late (>4 h) presentation treated by primary coronary angioplasty or thrombolytic therapy for acute myocardial infarction. Eur Heart J. 2002. 23:550–557.29. Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000. 283:2941–2947.30. Terkelsen CJ, Christiansen EH, Sorensen JT, Kristensen SD, Lassen JF, Thuesen L, Andersen HR, Vach W, Nielsen TT. Primary PCI as the preferred reperfusion therapy in STEMI: it is a matter of time. Heart. 2009. 95:362–369.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reperfusion Strategies in Acute ST-segment Elevation Myocardial Infarction
- ST segment
- Can time delay be shortened in the treatment of acute myocardial infarction?: Experience from Korea acute myocardial infarction registry
- Acute Myocardial Infarction by Right Coronary Artery Occlusion Presenting as Precordial ST Elevation on Electrocardiography
- Differences in Clinical Outcomes Between Patients With ST-Elevation Versus Non-ST-Elevation Acute Myocardial Infarction in Korea