J Korean Med Sci.
2010 Aug;25(8):1182-1186. 10.3346/jkms.2010.25.8.1182.
A Nationwide Survey of Lymphangioleiomyomatosis in Korea: Recent Increase in Newly Diagnosed Patients
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. mpchung@skku.edu
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Inha University Hospital, Inha University School of Medicine, Incheon, Korea.
- 3Division of Pulmonary Medicine, Department of Internal Medicine, Gachon Medical School Gil Medical Center, Incheon, Korea.
- 4Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea.
- 5Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University College of Medicine, and Lung Institute, Seoul National University Hospital, Seoul, Korea.
- 6Division of Respiration and Allergy Medicine, Soonchunhyang University Hospital, Seoul, Korea.
- 7Department of Internal Medicine, Bucheon Hospital, Soonchunhyang University School of Medicine, Bucheon, Korea.
- 8Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 9Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 10Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 11Department of Internal Medicine, Seoul Paik Hospital, Inje University, Seoul, Korea.
- 12Department of Internal Medicine, Hallym University College of Medicine, Kangdong Sacred Heart Hospital, Seoul, Korea.
- KMID: 1714040
- DOI: http://doi.org/10.3346/jkms.2010.25.8.1182
Abstract
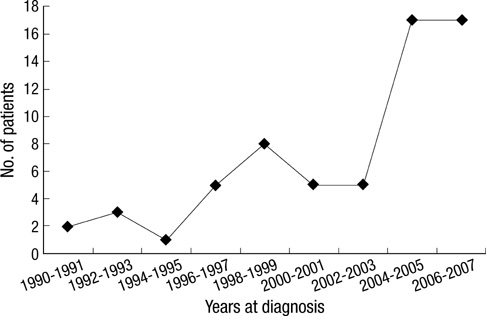
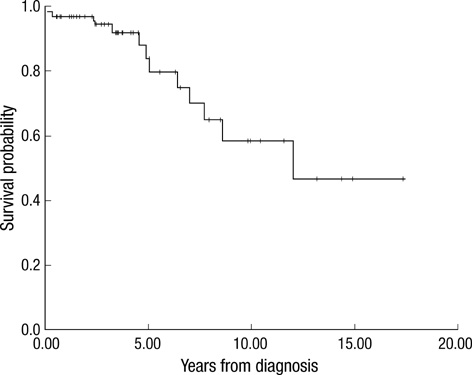
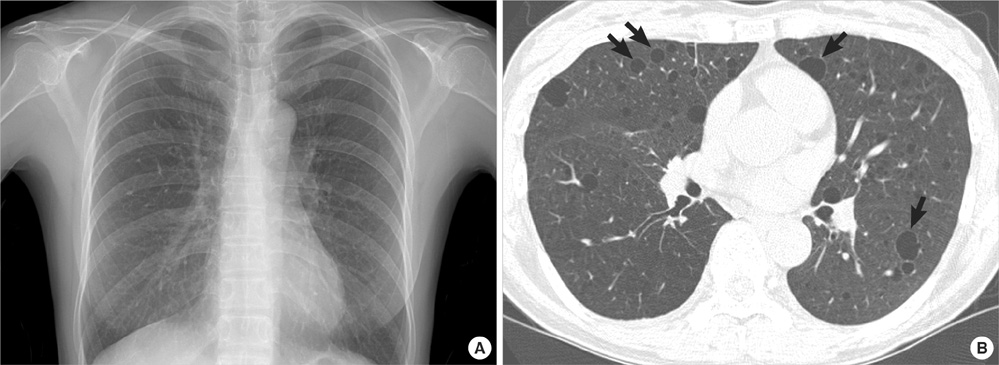
- In 2007, the Korean Interstitial Lung Disease Society had collected clinical data of patients who have diagnosed as Lymphangioleiomyomatosis (LAM) since 1990 through nationwide survey, which showed that LAM patients had increased sharply after 2004. The present study was performed to show the clinical features of Korean patients with LAM, and to establish the reason for the recent increase in the diagnosis. All 63 patients were women and the mean age at diagnosis was 36 yr. The most common presenting symptom was dyspnea and 8 patients had tuberous sclerosis complex. The survival rate at 5 yr after diagnosis was 84%. Compared with patients diagnosed after 2004 (n=34), the patients diagnosed before 2004 (n=29) complained with dyspnea more (P=0.016) and had lower FEV1% predicted (P=0.003), and DLco% predicted (P=0.042). The higher proportion of patients diagnosed after 2004 showed the normal chest radiography, and they were detected by routine chest CT screening (P=0.016). This study showed that clinical features of Korean patients with LAM were not different from those reported elsewhere. It is concluded that the reason for the increase of newly diagnosed patients is the result of increase in detection of the early stage LAM by the widespread use of chest CT screening.
MeSH Terms
Figure
Reference
-
1. Johnson SR. Lymphangioleiomyomatosis. Eur Respir J. 2006. 27:1056–1065.
Article2. Kitaichi M, Nishimura K, Itoh H, Izumi T. Pulmonary lymphangioleiomyomatosis: a report of 46 patients including a clinicopathologic study of prognostic factors. Am J Respir Crit Care Med. 1995. 151:527–533.
Article3. McCormack FX. Lymphangioleiomyomatosis: a clinical update. Chest. 2008. 133:507–516.4. Taylor JR, Ryu J, Colby TV, Raffin TA. Lymphangioleiomyomatosis. Clinical course in 32 patients. N Engl J Med. 1990. 323:1254–1260.5. Carrington CB, Cugell DW, Gaensler EA, Marks A, Redding RA, Schaaf JT, Tomasian A. Lymphangioleiomyomatosis. Physiologic-pathologic-radiologic correlations. Am Rev Respir Dis. 1977. 116:977–995.6. Eliasson AH, Phillips YY, Tenholder MF. Treatment of lymphangioleiomyomatosis. A meta-analysis. Chest. 1989. 96:1352–1355.7. Ryu JH, Moss J, Beck GJ, Lee JC, Brown KK, Chapman JT, Finlay GA, Olson EJ, Ruoss SJ, Maurer JR, Raffin TA, Peavy HH, McCarthy K, Taveira-Dasilva A, McCormack FX, Avila NA, Decastro RM, Jacobs SS, Stylianou M, Fanburg BL. The NHLBI lymphangioleiomyomatosis registry: characteristics of 230 patients at enrollment. Am J Respir Crit Care Med. 2006. 173:105–111.8. Urban T, Lazor R, Lacronique J, Murris M, Labrune S, Valeyre D, Cordier JF. Pulmonary lymphangioleiomyomatosis. A study of 69 patients. Groupe d'Etudes et de Recherche sur les Maladies "Orphelines" Pulmonaires (GERM"O"P). Medicine (Baltimore). 1999. 78:321–337.9. Chu SC, Horiba K, Usuki J, Avila NA, Chen CC, Travis WD, Ferrans VJ, Moss J. Comprehensive evaluation of 35 patients with lymphangioleiomyomatosis. Chest. 1999. 115:1041–1052.
Article10. Kalassian KG, Doyle R, Kao P, Ruoss S, Raffin TA. Lymphangioleiomyomatosis: new insights. Am J Respir Crit Care Med. 1997. 155:1183–1186.
Article11. Silverstein EF, Ellis K, Wolff M, Jaretzki A 3rd. Pulmonary lymphangiomyomatosis. Am J Roentgenol Radium Ther Nucl Med. 1974. 120:832–850.
Article12. Johnson SR, Tattersfield AE. Clinical experience of lymphangioleiomyomatosis in the UK. Thorax. 2000. 55:1052–1057.
Article13. Oh YM, Mo EK, Jang SH, Yoo CG, Kim YW, Seo JW, Han SK, Im JG, Shim YS. Pulmonary lymphangioleiomyomatosis in Korea. Thorax. 1999. 54:618–621.
Article14. Muller NL, Chiles C, Kullnig P. Pulmonary lymphangiomyomatosis: correlation of CT with radiographic and functional findings. Radiology. 1990. 175:335–339.
Article15. Bissler JJ, McCormack FX, Young LR, Elwing JM, Chuck G, Leonard JM, Schmithorst VJ, Laor T, Brody AS, Bean J, Salisbury S, Franz DN. Sirolimus for angiomyolipoma in tuberous sclerosis complex or lymphangioleiomyomatosis. N Engl J Med. 2008. 358:140–151.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrent Pneumothorax Caused by an Unexpected Lymphangioleiomyomatosis: A Case Report
- Anesthetic management for cesarean delivery in a patient with lymphangioleiomyomatosis: A case report
- Pulmonary Lymphangioleiomyomatosis with Chylous Pleural Effusion
- Pulmonary lymphangioleiomyomatosis: high-resolution CT findings
- A Case of Lymphangioleiomyomatosis Looked Like Miliary Tuberculosis