J Korean Med Sci.
2010 May;25(5):728-733. 10.3346/jkms.2010.25.5.728.
Early Vascular Access Blood Flow as a Predictor of Long-term Vascular Access Patency in Incident Hemodialysis Patients
- Affiliations
-
- 1Department of Internal Medicine, Gachon University of Medicine and Science, Incheon, Korea. imsejoong@hanmail.net
- 2Department of Surgery, Gachon University of Medicine and Science, Incheon, Korea.
- KMID: 1713957
- DOI: http://doi.org/10.3346/jkms.2010.25.5.728
Abstract
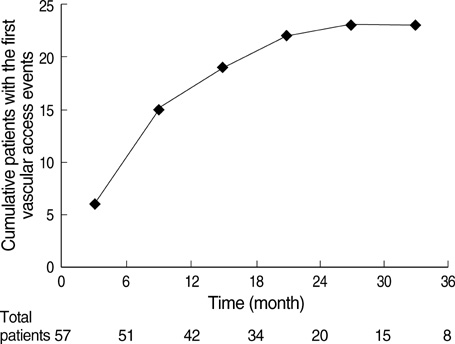
- The long-term clinical benefits of vascular access blood flow (VABF) measurements in hemodialysis (HD) patients have been controversial. We evaluated whether early VABF may predict long-term vascular access (VA) patency in incident HD patients. We enrolled 57 patients, of whom 27 were starting HD with arteriovenous fistulas (AVFs) and 30 with arteriovenous grafts (AVGs). The patients' VABF was measured monthly with the ultrasound dilution technique over the course of the first six months after the VA operation. During the 20.4-month observational period, a total of 40 VA events in 23 patients were documented. The new VA events included 13 cases of stenosis and 10 thrombotic events. The lowest quartile of average early VABF was related to the new VA events. After adjusting for covariates such as gender, age, hypertension, diabetes, VA type, hemoglobin levels, body mass index, parathyroid hormone, and calcium-phosphorus product levels, the hazard ratio of VABF (defined as <853 mL/min in AVF or <830 mL/min in AVG) to incident VA was 3.077 (95% confidence interval, 1.127-8.395; P=0.028). There were no significant relationships between early VABF parameters and VA thrombosis. It is concluded that early VABF may predict long-term VA patency, particularly VA stenosis.
MeSH Terms
-
Blood Vessel Prosthesis/*statistics & numerical data
Female
Graft Occlusion, Vascular/*diagnosis/*epidemiology
*Graft Survival
Humans
Indicator Dilution Techniques/statistics & numerical data
Kidney Function Tests/*statistics & numerical data
Korea/epidemiology
Male
Middle Aged
Prevalence
Prognosis
Renal Dialysis/*statistics & numerical data
Reproducibility of Results
Risk Assessment
Risk Factors
Sensitivity and Specificity
Treatment Outcome
*Vascular Patency
Figure
Reference
-
1. Vascular Access 2006 Work Group. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006. 48:Suppl 1. S248–S273.2. Tonelli M, James M, Wiebe N, Jindal K, Hemmelgarn B. Ultrasound monitoring to detect access stenosis in hemodialysis patients: a systematic review. Am J Kidney Dis. 2008. 51:630–640.
Article3. Hakim RM, Breyer J, Ismail N, Schulman G. Effects of dose of dialysis on morbidity and mortality. Am J Kidney Dis. 1994. 23:661–669.
Article4. Bosman PJ, Boereboom FT, Eikelboom BC, Koomans HA, Blankestijn PJ. Graft flow as a predictor of thrombosis in hemodialysis grafts. Kidney Int. 1998. 54:1726–1730.
Article5. Tessitore N, Bedogna V, Gammaro L, Lipari G, Poli A, Baggio E, Firpo M, Morana G, Mansueto G, Maschio G. Diagnostic accuracy of ultrasound dilution access blood flow measurement in detecting stenosis and predicting thrombosis in native forearm arteriovenous fistulae for hemodialysis. Am J Kidney Dis. 2003. 42:331–341.
Article6. Tessitore N, Lipari G, Poli A, Bedogna V, Baggio E, Loschiavo C, Mansueto G, Lupo A. Can blood flow surveillance and pre-emptive repair of subclinical stenosis prolong the useful life of arteriovenous fistulae? A randomized controlled study. Nephrol Dial Transplant. 2004. 19:2325–2333.
Article7. Neyra NR, Ikizler TA, May RE, Himmelfarb J, Schulman G, Shyr Y, Hakim RM. Change in access blood flow over time predicts vascular access thrombosis. Kidney Int. 1998. 54:1714–1719.
Article8. Schwab SJ, Oliver MJ, Suhocki P, McCann R. Hemodialysis arteriovenous access: detection of stenosis and response to treatment by vascular access blood flow. Kidney Int. 2001. 59:358–362.
Article9. Wang E, Schneditz D, Nepomuceno C, Lavarias V, Martin K, Morris AT, Levin NW. Predictive value of access blood flow in detecting access thrombosis. ASAIO J. 1998. 44:M555–M558.
Article10. May RE, Himmelfarb J, Yenicesu M, Knights S, Ikizler TA, Schulman G, Hernanz-Schulman M, Shyr Y, Hakim RM. Predictive measures of vascular access thrombosis: a prospective study. Kidney Int. 1997. 52:1656–1662.
Article11. Bosman PJ, Boereboom FT, Bakker CJ, Mali WP, Eikelboom BC, Blankestijn PJ, Koomans HA. Access flow measurements in hemodialysis patients: in vivo validation of an ultrasound dilution technique. J Am Soc Nephrol. 1996. 7:966–969.
Article12. Krivitski NM. Theory and validation of access flow measurement by dilution technique during hemodialysis. Kidney Int. 1995. 48:244–250.
Article13. Aruny JE, Lewis CA, Cardella JF, Cole PE, Davis A, Drooz AT, Grassi CJ, Gray RJ, Husted JW, Jones MT, McCowan TC, Meranze SG, Van Moore A, Neithamer CD, Oglevie SB, Omary RA, Patel NH, Rholl KS, Roberts AC, Sacks D, Sanchez O, Silverstein MI, Singh H, Swan TL, Towbin RB, Trerotola SO, Bakal CW. Quality improvement guidelines for percutaneous management of the thrombosed or dysfunctional dialysis access. J Vasc Interv Radiol. 2003. 14:S247–S253.
Article14. Papanikolaou V, Papagiannis A, Vrochides D, Imvrios G, Gakis D, Fouzas I, Antoniadis N, Takoudas D. The natural history of vascular access for hemodialysis: a single center study of 2,422 patients. Surgery. 2009. 145:272–279.
Article15. Moist LM, Churchill DN, House AA, Millward SF, Elliott JE, Kribs SW, DeYoung WJ, Blythe L, Stitt LW, Lindsay RM. Regular monitoring of access flow compared with monitoring of venous pressure fails to improve graft survival. J Am Soc Nephrol. 2003. 14:2645–2653.
Article16. Lindsay RM, Blake PG, Malek P, Posen G, Martin B, Bradfield E. Hemodialysis access blood flow rates can be measured by a differential conductivity technique and are predictive of access clotting. Am J Kidney Dis. 1997. 30:475–482.
Article17. Kim YO, Yang CW, Yoon SA, Chun KA, Kim NI, Park JS, Kim BS, Kim YS, Chang YS, Bang BK. Access blood flow as a predictor of early failures of native arteriovenous fistulas in hemodialysis patients. Am J Nephrol. 2001. 21:221–225.
Article18. Hoeben H, Abu-Alfa AK, Reilly RF, Aruny JE, Bouman K, Perazella MA. Vascular access surveillance: evaluation of combining dynamic venous pressure and vascular access blood flow measurements. Am J Nephrol. 2003. 23:403–408.
Article19. Saran R, Dykstra DM, Wolfe RA, Gillespie B, Held PJ, Young EW. Association between vascular access failure and the use of specific drugs: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2002. 40:1255–1263.
Article20. Schwarz C, Mitterbauer C, Boczula M, Maca T, Funovics M, Heinze G, Lorenz M, Kovarik J, Oberbauer R. Flow monitoring: performance characteristics of ultrasound dilution versus color Doppler ultrasound compared with fistulography. Am J Kidney Dis. 2003. 42:539–545.
Article21. Ha SJ, Lee YJ, Cho BH, Jung KH, Moon JY, Lee SH, Lee TW, Ihm CG. Glucose pump technique is as good as ultrasound dilution technique for vascular access surveillance in hemodialysis patients. Korean J Nephrol. 2007. 26:448–454.22. Lee KH, Park JY, Choi SJ, Kim JK, Hwang SD, Joh JH. Clinical utility of access blood flow measurement by ultrasound dilution in hemodialysis patients. Korean J Nephrol. 2005. 24:265–273.23. Shahin H, Reddy G, Sharafuddin M, Katz D, Franzwa BS, Dixon BS. Monthly access flow monitoring with increased prophylactic angioplasty did not improve fistula patency. Kidney Int. 2005. 68:2352–2361.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impacts of monthly arteriovenous fistula flow surveillance on hemodialysis access thrombosis and loss
- Risk Factors that Influence the Early Access Patency of an Arteriovenous Fistula in Hemodialysis Patients
- Impact of monthly arteriovenous fistula flow surveillance on hemodialysis access thrombosis and loss
- The Patency Rate of Hemodialysis Vascular Access and the Analysis of Patency-related Factors: Comparision of Native Arteriovenous Fistula with Arteriovenous Graft, Single Center Study
- History and Development of Vascular Access and Its Impact on Hemodialysis Outcome