J Korean Med Sci.
2010 May;25(5):691-697. 10.3346/jkms.2010.25.5.691.
Efficacy of Tandem High-Dose Chemotherapy and Autologous Stem Cell Rescue in Patients Over 1 Year of Age with Stage 4 Neuroblastoma: The Korean Society of Pediatric Hematology-Oncology Experience Over 6 Years (2000-2005)
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Pediatrics, Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Pediatrics, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 4Department of Pediatrics, Kyung Hee University Medical Center, Kyung Hee University College of Medicine, Seoul, Korea.
- 5Department of Pediatrics, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea.
- 6Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 7Division of Pediatric Hematology and Oncology, Department of Pediatrics, Severance Hospital, Yonsei University Health System, Seoul, Korea.
- 8Department of Pediatrics8, Kyungpook National University Hospital, Kyungpook National University School of Medicine, Daegu, Korea. kslee@knu.ac.kr
- KMID: 1713951
- DOI: http://doi.org/10.3346/jkms.2010.25.5.691
Abstract
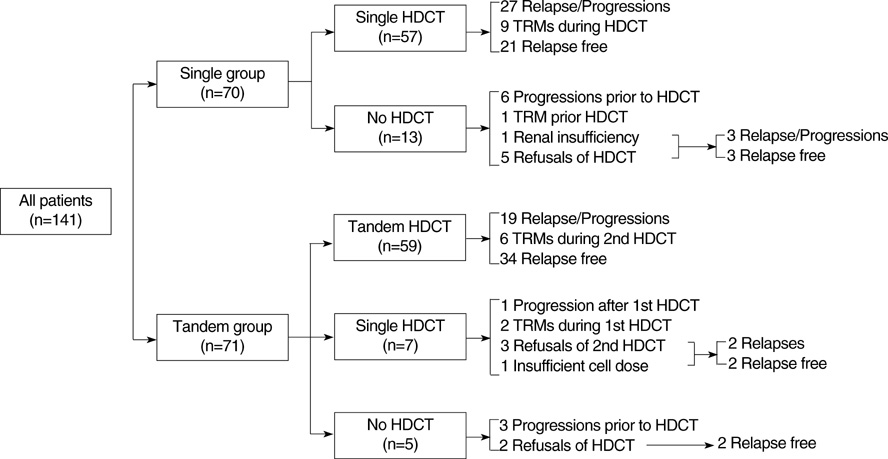
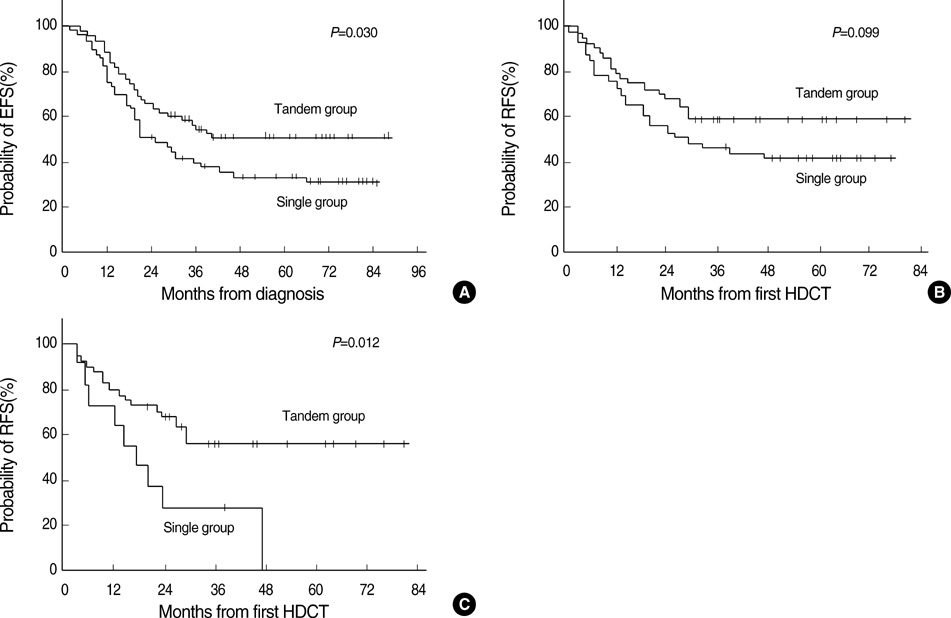
- The efficacy of tandem high-dose chemotherapy and autologous stem cell rescue (HDCT/ASCR) was investigated in patients with high-risk neuroblastoma. Patients over 1 yr of age who were newly diagnosed with stage 4 neuroblastoma from January 2000 to December 2005 were enrolled in The Korean Society of Pediatric Hematology-Oncology registry. All patients who were assigned to receive HDCT/ASCR at diagnosis were retrospectively analyzed to investigate the efficacy of single or tandem HDCT/ASCR. Seventy and 71 patients were assigned to receive single or tandem HDCT/ASCR at diagnosis. Fifty-seven and 59 patients in the single or tandem HDCT group underwent single or tandem HDCT/ASCR as scheduled. Twenty-four and 38 patients in the single or tandem HDCT group remained event free with a median follow-up of 56 (24-88) months. When the survival rate was analyzed according to intent-to-treat at diagnosis, the probability of the 5-yr event-free survival+/-95% confidence intervals was higher in the tandem HDCT group than in the single HDCT group (51.2+/-12.4% vs. 31.3+/-11.5%, P=0.030). The results of the present study demonstrate that the tandem HDCT/ASCR strategy is significantly better than the single HDCT/ASCR strategy for improved survival in the treatment of high-risk neuroblastoma patients.
MeSH Terms
-
Adolescent
Child
Child, Preschool
Combined Modality Therapy/mortality
Drug Therapy/*mortality
Female
Humans
Infant
Korea/epidemiology
Longitudinal Studies
Male
Neuroblastoma/*mortality/*therapy
Prevalence
Risk Assessment/methods
Risk Factors
Stem Cell Transplantation/*mortality
Survival Analysis
Survival Rate
Treatment Outcome
Figure
Reference
-
1. Frappaz D, Michon J, Coze C, Berger C, Plouvier E, Lasset C, Bernard JL, Stephan JL, Bouffet E, Buclon M, Combaret V, Fourquet A, Philip T, Zucker JM. LMCE3 treatment strategy: results in 99 consecutively diagnosed stage 4 neuroblastomas in children older than 1 year at diagnosis. J Clin Oncol. 2000. 18:468–476.
Article2. Stram DO, Matthay KK, O'Leary M, Reynolds CP, Haase GM, Atkinson JB, Brodeur GM, Seeger RC. Consolidation chemoradiotherapy and autologous bone marrow transplantation versus continued chemotherapy for metastatic neuroblastoma: a report of two concurrent Children's Cancer Group studies. J Clin Oncol. 1996. 14:2417–2426.
Article3. Matthay KK, Villablanca JG, Seeger RC, Stram DO, Harris RE, Ramsay NK, Swift P, Shimada H, Black CT, Brodeur GM, Gerbing RB, Reynolds CP. Children's Cancer Group. Treatment of high-risk neuroblastoma with intensive chemotherapy, radiotherapy, autologous bone marrow transplantation, and 13-cis-retinoic acid. N Engl J Med. 1999. 341:1165–1173.
Article4. Ladenstein R, Philip T, Lasset C, Hartmann O, Garaventa A, Pinkerton R, Michon J, Prichard J, Klingebiel T, Kremens B, Pearson A, Coze C, Paolucci P, Frappaz D, Gadner H, Chauvin F. Multivariate analysis of risk factors in stage 4 neuroblastoma patients over the age of one year treated with megatherapy and stem-cell transplantation: a report from the European Bone Marrow Transplantation Solid Tumor Registry. J Clin Oncol. 1998. 16:953–965.
Article5. Cohn SL, Moss TJ, Hoover M, Katzenstein HM, Haut PR, Morgan ER, Green AA, Kletzel M. Treatment of poor-risk neuroblastoma patients with high-dose chemotherapy and autologous peripheral stem cell rescue. Bone Marrow Transplant. 1997. 20:543–551.
Article6. Berthold F, Boos J, Burdach S, Erttmann R, Henze G, Hermann J, Klingebiel T, Kremens B, Schilling FH, Schrappe M, Simon T, Hero B. Myeloablative megatherapy with autologous stem-cell rescue versus oral maintenance chemotherapy as consolidation treatment in patients with high-risk neuroblastoma: a randomized controlled trial. Lancet Oncol. 2005. 6:649–658.7. George RE, Li S, Medeiros-Nancarrow C, Neuberg D, Marcus K, Shamberger RC, Pulsipher M, Grupp SA, Diller L. High-risk neuroblastoma treated with tandem autologous peripheral-blood stem cell-supported transplantation: long-term survival update. J Clin Oncol. 2006. 24:2891–2896.
Article8. Sung KW, Lee SH, Yoo KH, Jung HL, Cho EJ, Koo HH, Lee SK, Kim J, Lim DH, Suh YL, Kim DW. Tandem high-dose chemotherapy and autologous stem cell rescue in patients over 1 year of age with stage 4 neuroblastoma. Bone Marrow Transplant. 2007. 40:37–45.
Article9. Kletzel M, Katzenstein HM, Haut PR, Yu AL, Morgan E, Reynolds M, Geissler G, Marymount MH, Liu D, Kalapurakal JA, Shore RM, Bardo DM, Schmoldt J, Rademaker AW, Cohn SL. Treatment of high-risk neuroblastoma with triple-tandem high-dose therapy and stem-cell rescue: results of the Chicago Pilot II Study. J Clin Oncol. 2002. 20:2284–2292.
Article10. Brodeur GM, Pritchard J, Berthold F, Carlsen NL, Castel V, Castelberry RP, De Bernardi B, Evans AE, Favrot M, Hedborg F. Revisions of the international criteria for neuroblastoma diagnosis, staging, and response to treatment. J Clin Oncol. 1993. 11:1466–1477.
Article11. Flandin I, Hartmann O, Michon J, Pinkerton R, Coze C, Stephan JL, Fourquet B, Valteau-Couanet D, Bergeron C, Philip T, Carrie C. Impact of TBI on late effects in children treated by megatherapy for Stage IV neuroblastoma. A study of the French Society of Pediatric oncology. Int J Radiat Oncol Biol Phys. 2006. 64:1424–1431.
Article12. Meacham LR, Gurney JG, Mertens AC, Ness KK, Sklar CA, Robison LL, Oeffinger KC. Body mass index in long-term adult survivors of childhood cancer: a report of the Childhood Cancer Survivor Study. Cancer. 2005. 103:1730–1739.13. Hobbie WL, Moshang T, Carlson CA, Goldmuntz E, Sacks N, Goldfarb SB, Grupp SA, Ginsberg JP. Late effects in survivors of tandem peripheral blood stem cell transplant for high-risk neuroblastoma. Pediatr Blood Cancer. 2008. 51:679–683.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Autologous Cord Blood Stem Cell Transplantationin Stage IV Neuroblastoma
- High-dose Chemotherapy and Autologous Stem Cell Rescue in Patients with High-risk Stage 3 Neuroblastoma: 10-Year Experience at a Single Center
- Improved Survival in Neuroblastoma by Autologous Peripheral Blood Stem Cell Transplantation: A Single Institution Experience
- Treatment outcomes of high-dose chemotherapy plus stem cell rescue in high-risk neuroblastoma patients in Thailand
- Successful Response of Oral Etoposide for Refractory Neuroblastoma