J Korean Med Sci.
2008 Apr;23(2):350-354. 10.3346/jkms.2008.23.2.350.
Catastrophic Catecholamine-Induced Cardiomyopathy Mimicking Acute Myocardial Infarction, Rescued by Extracorporeal Membrane Oxygenation (ECMO) in Pheochromocytoma
- Affiliations
-
- 1Department of Medicine, Division of Cardiology, Asan Medical Center, University of Ulsan, Seoul, Korea. sjpark@amc.seoul.kr
- 2Department of Cardiothoracic Surgery, Asan Medical Center, University of Ulsan, Seoul, Korea.
- KMID: 1713475
- DOI: http://doi.org/10.3346/jkms.2008.23.2.350
Abstract
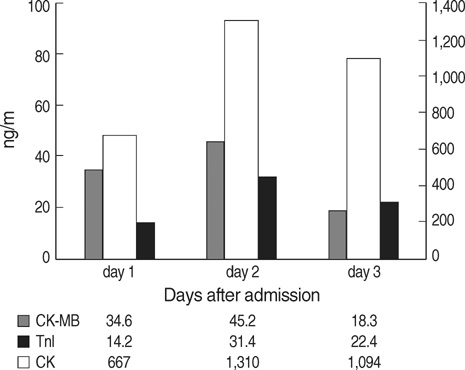
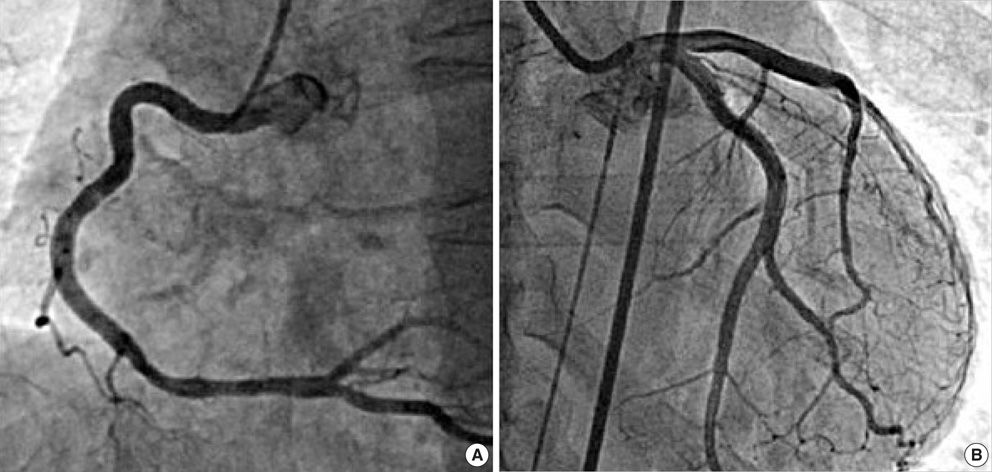
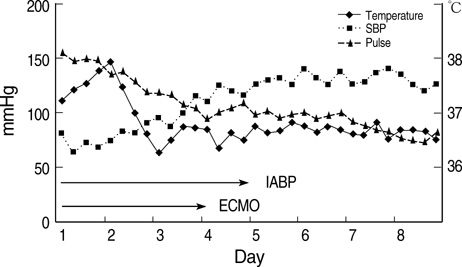
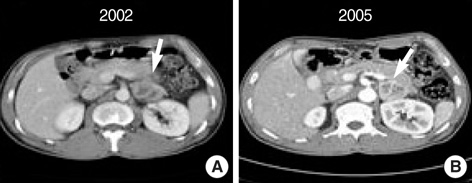
- Pheochromocytoma is a rare disorder and functioning tumor composed of chromaffin cells that secrete catecholamines. Patients with a pheochromocytoma 'crisis' have a high mortality in spite of aggressive therapy. We present a case with a severe acute catecholamine cardiomyopathy presenting ST segment elevation with cardiogenic shock after hemorrhage into a left suprarenal tumor. Intra-aortic balloon pump (IABP) support, combined with inotropic therapy, was performed. However, the patient deteriorated rapidly and was unresponsive to a full dose of inotropics and IABP. We decided to apply extracorporeal membrane oxygenation (ECMO) device for the patient. His clinical state began to improve 3 days after ECMO. After achieving hemodynamic stabilization, he underwent successful laparoscopic left adrenalectomy. He needed no further cardiac medication after discharge.
Keyword
MeSH Terms
-
Adrenal Glands/pathology
Adult
Cardiomyopathies/*diagnosis/*etiology
Catecholamines/*adverse effects
Coronary Angiography/methods
Diagnosis, Differential
Electrocardiography/methods
Extracorporeal Membrane Oxygenation/*methods
Humans
Intra-Aortic Balloon Pumping
Male
Myocardial Infarction/*diagnosis
Pheochromocytoma/*therapy
Time Factors
Tomography, X-Ray Computed/methods
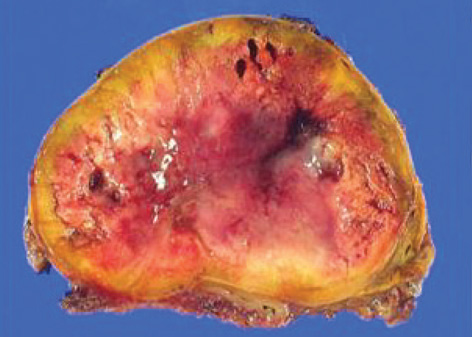
Figure
Cited by 2 articles
-
Catecholamine-Induced Cardiomyopathy associated with Neuroblastoma and Treated with Extracorporeal Membrane Oxygenation as a Bridge to Recovery
Junggu Yi, Si Oh Kim, Jun-mo Park, Sung-hye Byun, Hoon Jung, Seong Wook Hong
Korean J Crit Care Med. 2015;30(4):299-302. doi: 10.4266/kjccm.2015.30.4.299.Catastrophic catecholamine-induced cardiomyopathy rescued by extracorporeal membrane oxygenation in recurrent malignant pheochromocytoma
Daniel Min
Yeungnam Univ J Med. 2019;36(3):254-259. doi: 10.12701/yujm.2019.00213.
Reference
-
1. Lenders JW, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet. 2005. 366:665–675.
Article2. Plouin PF, Degoulet P, Tugayé A, Ducrocq MB, Ménard J. [Screening for phaeochromocytoma: in which hypertensive patients? A semiological study of 2585 patients, including 11 with phaeochromocytoma (author's transl). Nouv Presse Med. 1981. 10:869–872.3. Schifferdecker B, Kodali D, Hausner E, Aragam J. Adrenergic shock-an overlooked clinical entity? Cardiol Rev. 2005. 13:69–72.4. Sardesai SH, Mourant AJ, Sivathandon Y, Farrow R, Gibbons DO. Phaeochromocytoma and catecholamine induced cardiomyopathy presenting as heart failure. Br Heart J. 1990. 63:234–237.
Article5. Huddle KR, Kalliatakis B, Skoularigis J. Pheochromocytoma associated with clinical and echocardiographic features simulating hypertrophic obstructive cardiomyopathy. Chest. 1996. 109:1394–1397.
Article6. Gupta KK. Letter: Phaeochromocytoma and myocardial infarction. Lancet. 1975. 1:281–282.7. Nirgiotis JG, Andrassy RJ. Pheochromocytoma and acute myocardial infarction. South Med J. 1990. 83:1478–1480.
Article8. Szakacs JE, Cannon A. L-Norepinephrine myocarditis. Am J Clin Pathol. 1958. 30:425–434.
Article9. Kline IK. Myocardial alterations associated with pheochromocytomas. Am J Pathol. 1961. 38:539–551.10. Seeley E WG. The heart in endocrine disorders. Braunwald's heart disease: a textbook of cardiovascular medicine. 2005. 7th ed. New York: W.B. Saunders Co.;2063–2064. .11. Sayer WJ, Moser M, Mattingly TW. Pheochromocytoma and the abnormal electrocardiogram. Am Heart J. 1954. 48:42–53.
Article12. Shimizu K, Miura Y, Meguro Y, Noshio T, Ohzeki T, Kusakari T, Akama H, Watanabe T, Honma H, Imai Y. QT prolongation with torsade de pointes in pheochromocytoma. Am Heart J. 1992. 124:235–239.
Article13. Haas GJ, Tzagournis M, Boudoulas H. Pheochromocytoma: catecholamine-mediated electrocardiographic changes mimicking ischemia. Am Heart J. 1988. 116:1363–1365.
Article14. Cheng TO, Bashour TT. Striking electrocardiographic changes associated with pheochromocytoma. Masquerading as ischemic heart disease. Chest. 1976. 70:397–399.15. McManus BM, Fleury TA, Roberts WC. Fatal catecholamine crisis in pheochromocytoma: curable cause of cardiac arrest. Am Heart J. 1981. 102:930–932.
Article16. Delaney JP, Paritzky AZ. Necrosis of a pheochromocytoma with shock. N Engl J Med. 1969. 280:1394–1395.
Article17. Duh QY. Evolving surgical management for patients with pheochromocytoma. J Clin Endocrinol Metab. 2001. 86:1477–1479.
Article18. Dembitsky WP, Moreno-Cabral RJ, Adamson RM, Daily PO. Emergency resuscitation using portable extracorporeal membrane oxygenation. Ann Thorac Surg. 1993. 55:304–309.
Article19. Chen YS, Wang MJ, Chou NK, Han YY, Chiu IS, Lin FY, Chu SH, Ko WJ. Rescue for acute myocarditis with shock by extracorporeal membrane oxygenation. Ann Thorac Surg. 1999. 68:2220–2224.
Article20. Takagi S, Miyazaki S, Fujii T, Daikoku S, Sutani Y, Morii I, Yasuda S, Goto Y, Nonogi H. Dexamethasone-induced cardiogenic shock rescued by percutaneous cardiopulmonary support (PCPS) in a patient with pheochromocytoma. Jpn Circ J. 2000. 64:785–788.
Article21. Shen WT, Sturgeon C, Clark OH, Duh QY, Kebebew E. Should pheochromocytoma size influence surgical approach? A comparison of 90 malignant and 60 benign pheochromocytomas. Surgery. 2004. 136:1129–1137.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Catastrophic catecholamine-induced cardiomyopathy rescued by extracorporeal membrane oxygenation in recurrent malignant pheochromocytoma
- Catecholamine-Induced Cardiomyopathy associated with Neuroblastoma and Treated with Extracorporeal Membrane Oxygenation as a Bridge to Recovery
- Successful extracorporeal membrane oxygenation treatment of catecholamine-induced cardiomyopathy-associated pheochromocytoma: a case report
- Extracorporeal Membrane Oxygenation for 67 Days as a Bridge to Heart Transplantation in a Postcardiotomy Patient with Failing Heart and Mediastinitis
- Delayed Repair of Ventricular Septal Rupture Following Preoperative Awake Extracorporeal Membrane Oxygenation Support