J Korean Med Sci.
2007 Feb;22(1):74-80. 10.3346/jkms.2007.22.1.74.
Impact of Clinical Characteristics of Individual Metabolic Syndrome on the Severity of Insulin Resistance in Chinese Adults
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Tri-Service General Hospital, Taipei, Taiwan, R.O.C.
- 2Xindian Buddhist Tzu Chi General Hospital, No 289 Jianguo Rd, Xiandian City, Taipei County, Taiwan, R.O.C. peidee@gmail.com
- 3Veterans General Hospital, Taichung, Taiwan, R.O.C.
- 4Division of Family Practice, Buddhist Tzu Chi General Hospital, Xiandian, Taiwan, R.O.C.
- KMID: 1713233
- DOI: http://doi.org/10.3346/jkms.2007.22.1.74
Abstract
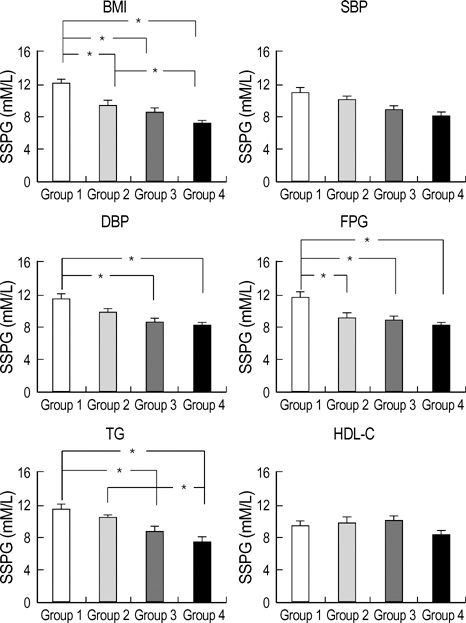
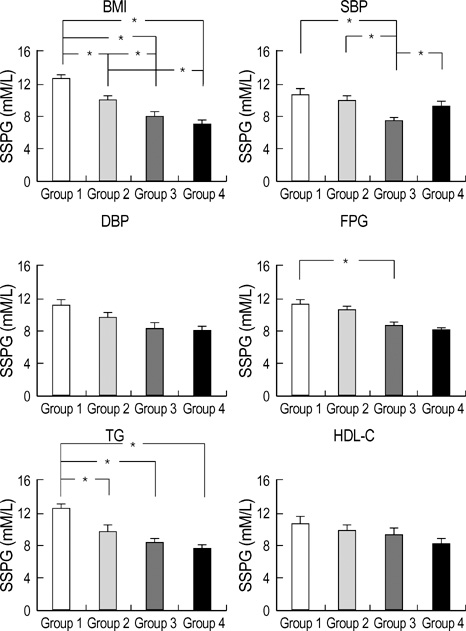
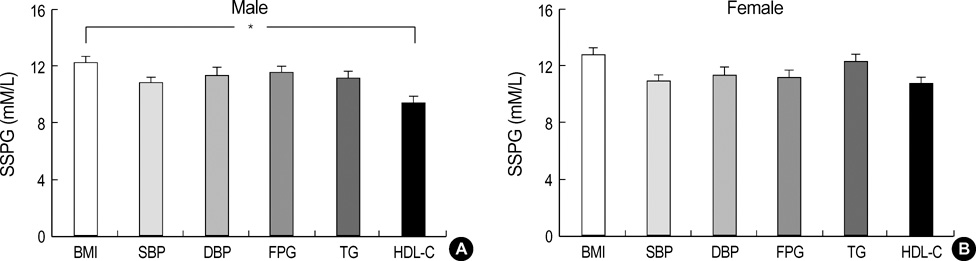
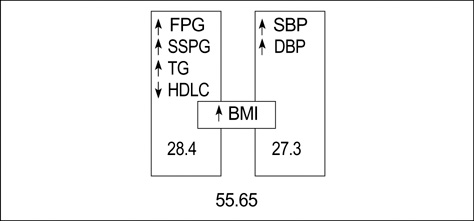
- The impact the metabolic syndrome (MetS) components on the severity of insulin resistance (IR) has not been reported. We enrolled 564 subjects with MetS and they were divided into quartiles according to the level of each component; and an insulin suppression test was performed to measure IR. In males, steady state plasma glucose (SSPG) levels in the highest quartiles, corresponding to body mass index (BMI) and fasting plasma glucose (FPG), were higher than the other three quartiles and the highest quartiles, corresponding to the diastolic blood pressure and triglycerides, were higher than in the lowest two quartiles. In females, SSPG levels in the highest quartiles, corresponding to the BMI and triglycerides, were higher than in all other quartiles. No significant differences existed between genders, other than the mean SSPG levels in males were greater in the highest quartile corresponding to BMI than that in the highest quartile corresponding to HDL-cholesterol levels. The factor analysis identified two underlying factors (IR and blood pressure factors) among the MetS variables. The clustering of the SSPG, BMI, triglyceride and HDLcholesterol was noted. Our data suggest that adiposity, higher FPG and triglyceride levels have stronger correlation with IR and subjects with the highest BMI have the highest IR.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Ketonuria after Fasting may be Related to the Metabolic Superiority
Nam-Seok Joo, Duck-Joo Lee, Kwang-Min Kim, Bom-Taeck Kim, Chan-Won Kim, Kyu-Nam Kim, Sang-Man Kim
J Korean Med Sci. 2010;25(12):1771-1776. doi: 10.3346/jkms.2010.25.12.1771.
Reference
-
1. Avogaro P, Crepaldi G, Enzi G, Tiengo A. Associazione di iperlipidemia, diabete mellito e obesita di medio grado. Acta Diabetol Lat. 1967. 4:36–41.2. Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988. 37:1595–1607.
Article3. Reaven GM. Role of insulin resistance in human disease (syndrome X): an expanded definition. Annu Rev Med. 1993. 44:121–131.
Article4. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998. 15:539–553.
Article5. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.6. Haffner SM, Valdez RA, Hazuda HP, Mitchell BD, Morales PA, Stern MP. Prospective analysis of the insulin-resistance syndrome (syndrome X). Diabetes. 1992. 41:715–722.
Article7. Zimmet PZ. Kelly West Lecture 1991, Challenges in diabetes epidemiology--from West to the rest. Diabetes Care. 1992. 15:232–252.
Article8. Meigs JB. Invited commentary: insulin resistance syndrome? Syndrome X? Multiple metabolic syndrome? A syndrome at all? Factor analysis reveals patterns in the fabric of correlated metabolic risk factors. Am J Epidemiol. 2000. 152:908–911.
Article9. Edwards KL, Austin MA, Newman B, Mayer E, Krauss RM, Selby JV. Multivariate analysis of the insulin resistance syndrome in women. Arterioscler Thromb. 1994. 14:1940–1945.
Article10. Shen SW, Reaven GM, Farquhar GW. Comparison of impedance to insulin-mediated glucose uptake in normal subjects and in subjects with latent diabetes. J Clin Invest. 1970. 49:2151–2160.
Article11. Herbert V, Lau KS, Gottlieb CW, Bleicher SJ. Coated charcoal immunoassay of insulin. J Clin Endocrinol Metab. 1965. 25:1375–1384.
Article12. Cureton EE, D'Agostino RB. Factor Analysis: An Applied Approach. 1983. Hilside, NJ: Lawrence Erlbaum.13. Meigs JB, D'Agostino RB, Wilson PW, Cupples LA, Nathan DM, Singer DE. Risk variable clustering in the insulin resistance syndrome: the Framingham Offspring Study. Diabetes. 1997. 46:1594–1600.
Article14. Cheal KL, Abbasi F, Lamendola C, McLaughlin T, Reaven GM, Ford ES. Relationship to insulin resistance of the adult treatment panel III diagnostic criteria for identification of the metabolic syndrome. Diabetes. 2004. 53:1195–1200.
Article15. Kissebah AH, Vydelingu N, Murray R, Evans DJ, Hartz AJ, Kalkhoff RK, Adams PW. Relation of body fat distribution to metabolic complications of obesity. J Clin Endocrinol Metab. 1982. 54:254–260.
Article16. Krotkiewski M, Bjorntorp P, Sjostrom L, Smith U. Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J Clin Invest. 1983. 72:1150–1162.
Article17. Ferrannini E, Natali A, Capaldo B, Lehtovirta M, Jacob S, Yki-Jarvinen H. Insulin resistance, hyperinsulinemia, and blood pressure: role of age and obesity. European Group for the Study of Insulin Resistance (EGIR). Hypertension. 1997. 30:1144–1149.18. Evans DJ, Murray R, Kissebah AH. Relationship between skeletal muscle insulin resistance, insulin-mediated glucose disposal, and insulin binding. Effects of obesity and body fat topography. J Clin Invest. 1984. 74:1515–1525.
Article19. Fujioka S, Matsuzawa Y, Tokunaga K, Tarui S. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism. 1987. 36:54–59.
Article20. Leenen R, van der Kooy K, Seidell JC, Deurenberg P. Visceral fat accumulation measured by magnetic resonance imaging in relation to serum lipids in obese men and women. Atherosclerosis. 1992. 94:171–181.
Article21. Ferrannini E, Buzzigoli G, Bonadonna R, Giorico MA, Oleggini M, Graziadei L, Pedrinelli R, Brandi L, Bevilacqua S. Insulin resistance in essential hypertension. N Engl J Med. 1987. 317:350–357.
Article22. Pollare T, Lithell H, Berne C. Insulin resistance is a characteristic feature of primary hypertension independent of obesity. Metabolism. 1990. 39:167–174.
Article23. Garg A, Helderman JH, Koffler M, Ayuso R, Rosenstock J, Raskin P. Relationship between lipoprotein levels and in vivo insulin action in normal young white men. Metabolism. 1988. 37:982–987.
Article24. Mykkanen L, Haffner SM, Ronnemaa T, Bergman R, Leino A, Laakso M. Is there a sex difference in the association of plasma insulin level and insulin sensitivity with serum lipids and lipoproteins? Metabolism. 1994. 43:523–528.
Article25. Abbott WG, Lillioja S, Young AA, Zawadzki JK, Yki-Jarvinen H, Christin L, Howard BV. Relationships between plasma lipoprotein concentrations and insulin action in an obese hyperinsulinemic population. Diabetes. 1987. 36:897–904.
Article26. Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003. 157:821–827.27. Perseghin G, Scifo P, Pagliato E, Battezzati A, Benedini S, Soldini L, Testolin G, Del Maschio A, Luzi L. Gender factors affect fatty acids-induced insulin resistance in nonobese humans: effects of oral steroidal contraception. J Clin Endocrinol Metab. 2001. 86:3188–3196.
Article28. Freedman DS, Jacobsen SJ, Barboriak JJ, Sobocinski KA, Anderson AJ, Kissebah AH, Sasse EA, Gruchow HW. Body fat distribution and male/female differences in lipids and lipoproteins. Circulation. 1990. 81:1498–1506.
Article29. Lemieux S, Despres JP, Moorjani S, Nadeau A, Theriault G, Prud'homme D, Tremblay A, Bouchard C, Lupien PJ. Are gender differences in cardiovascular disease risk factors explained by the level of visceral adipose tissue? Diabetologia. 1994. 37:757–764.
Article30. Saad MF, Rewers M, Selby J, Howard G, Jinagouda S, Fahmi S, Zaccaro D, Bergman RN, Savage PJ, Haffner SM. Insulin resistance and hypertension: the Insulin Resistance Atherosclerosis study. Hypertension. 2004. 43:1324–1331.31. Toft I, Bonaa KH, Jenssen T. Insulin resistance in hypertension is associated with body fat rather than blood pressure. Hypertension. 1998. 32:115–122.
Article32. Peiris AN, Struve MF, Kissebah AH. Relationship of body fat distribution to the metabolic clearance of insulin in premenopausal women. Int J Obes. 1987. 11:581–589.33. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985. 28:412–419.34. Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, Monauni T, Muggeo M. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care. 2000. 23:57–63.
Article35. Hollenbeck C, Reaven GM. Variations in insulin-stimulated glucose uptake in healthy individuals with normal glucose tolerance. J Clin Endocrinol Metab. 1987. 64:1169–1173.
Article36. Chen W, Srinivasan SR, Elkasabany A, Berenson GS. Cardiovascular risk factors clustering features of insulin resistance syndrome (Syndrome X) in a biracial (Black-White) population of children, adolescences, and young adults: the Bogalusa Heart Study. Am J Epidemiol. 1999. 150:667–674.37. Edwards KL, Burchfiel CM, Sharp DS, Curb JD, Rodriguez BL, Fujimoto WY, LaCroix AZ, Vitiello MV, Austin MA. Factors of the insulin resistance in nondiabetic and diabetic elderly Japaneses-American men. Am J Epidemiol. 1998. 147:441–447.38. Gray RS, Fabsitz RR, Cowan LD, Lee ET, Howard BV, Savage PJ. Risk factor clustering in the insulin resistance syndrome. The Strong Heart Study. Am J Epidemiol. 1998. 148:869–878.
Article39. Snehalatha C, Sivasankari S, Satyavani K, Vijay V, Ramachandran A. Insulin resistance alone dose not explain the clustering of cardiovascular risk factors in southern India. Diabet Med. 2000. 17:152–157.40. Hanley AJ, Karter AJ, Festa A, D'Agostino R Jr, Wagenknecht LE, Savage P, Tracy RP, Saad MF, Haffner S. Insulin Resistance Atherosclerosis Study. Factor analysis of metabolic syndrome using directly measured insulin sensitivity: The Insulin Resistance Atherosclerosis Study. Diabetes. 2002. 51:2642–2647.
Article