Korean J Radiol.
2013 Dec;14(6):905-913. 10.3348/kjr.2013.14.6.905.
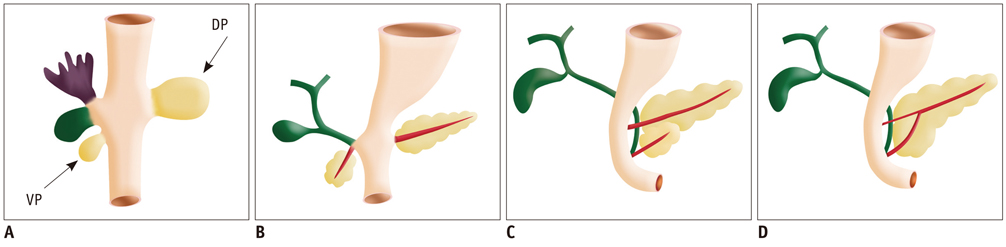
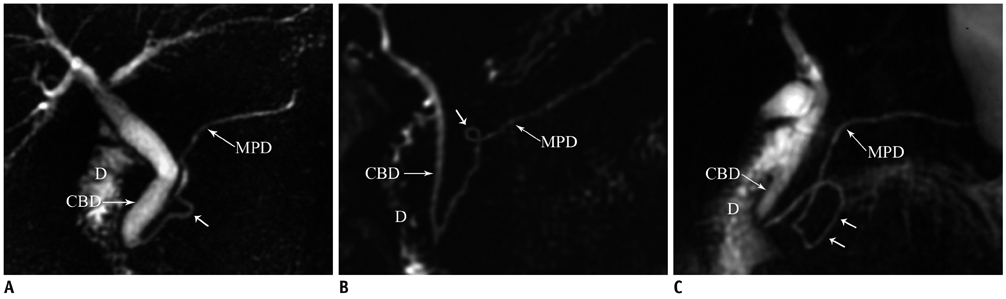
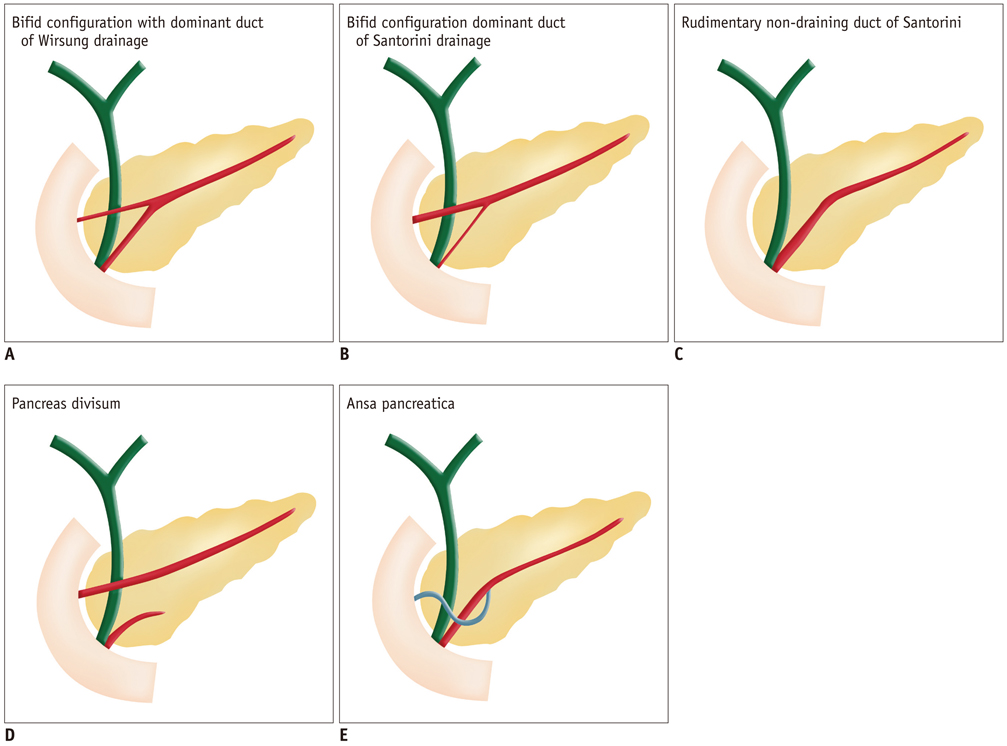
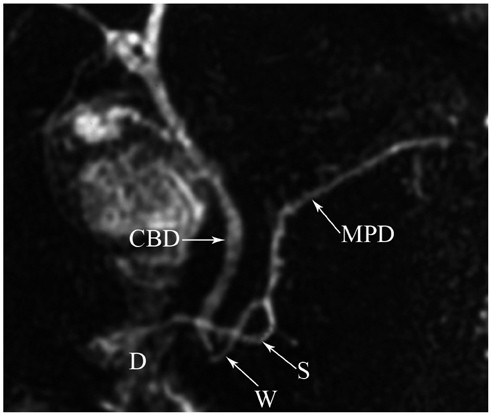
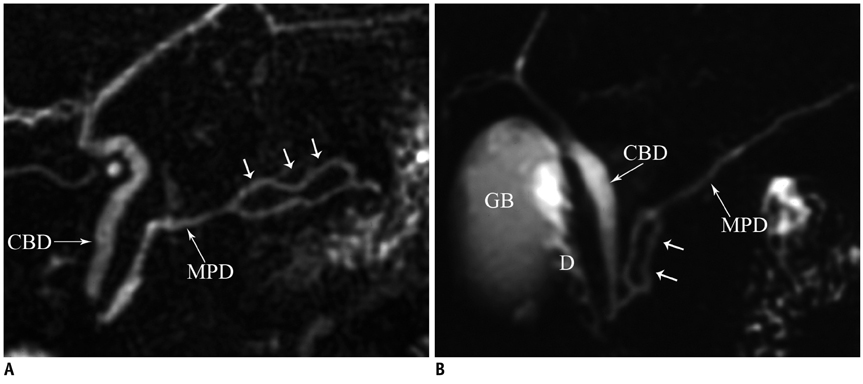
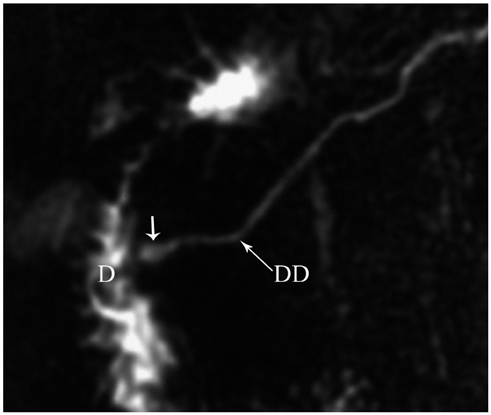
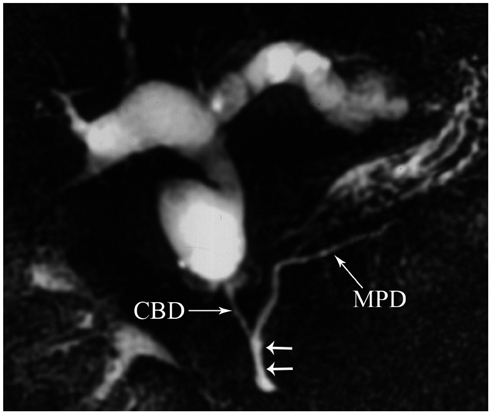
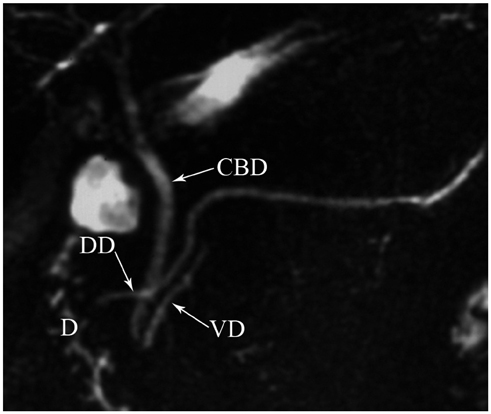
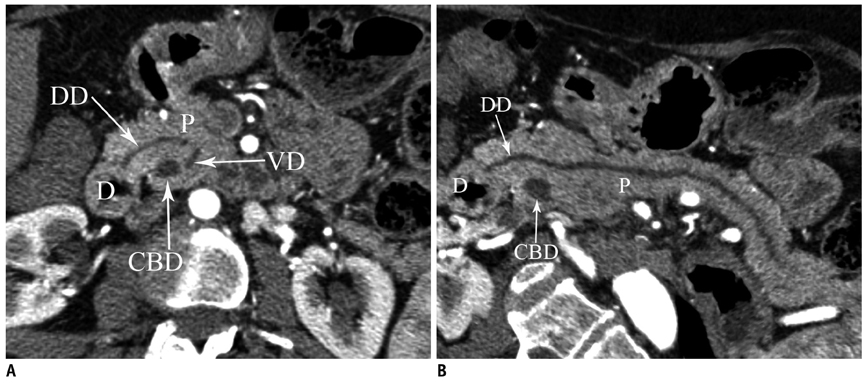
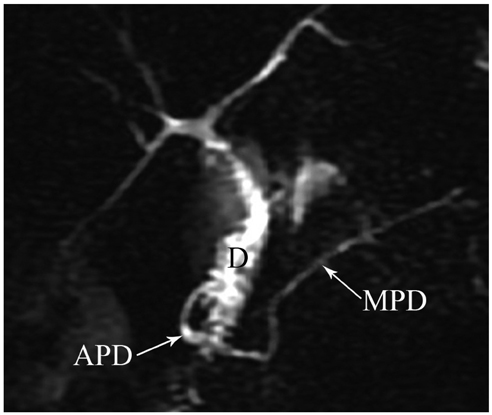
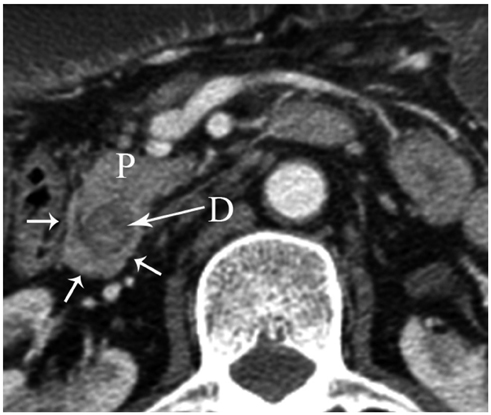
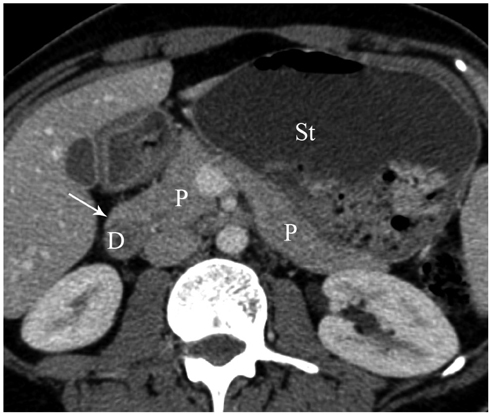
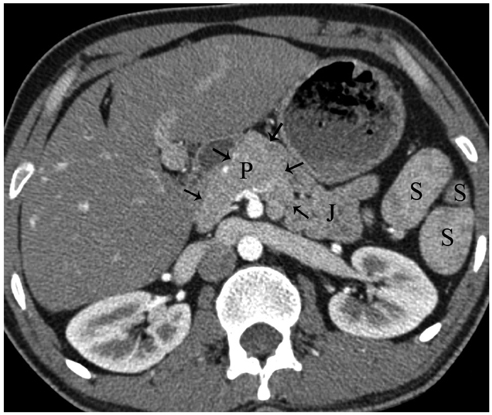
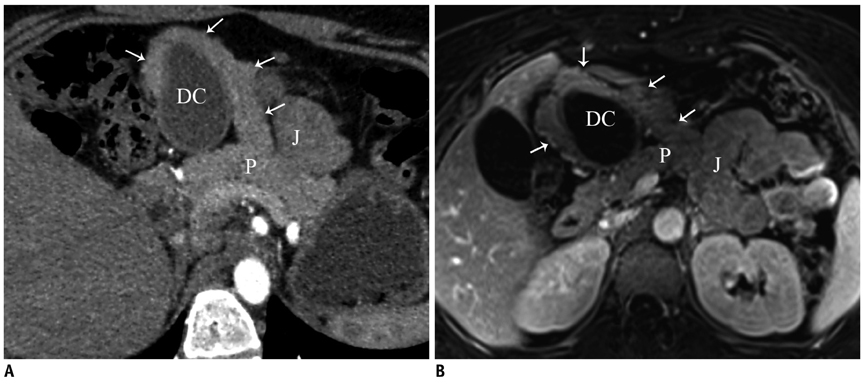
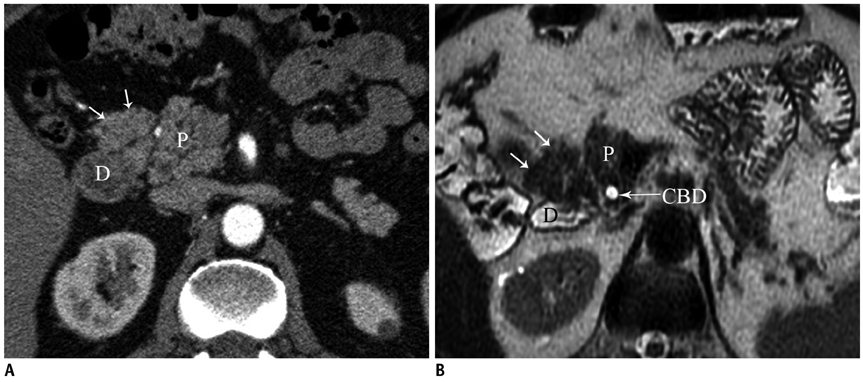
Congenital Variants and Anomalies of the Pancreas and Pancreatic Duct: Imaging by Magnetic Resonance Cholangiopancreaticography and Multidetector Computed Tomography
- Affiliations
-
- 1Department of Radiology, Turkiye Yuksek Ihtisas Hospital, Kizilay street, No:4, 06100, Sihhiye, Ankara, Turkey. aturkvatan@yahoo.com
- 2Department of Radiology, Ankara University School of Medicine, Talatpasa Street, 06100, Sihhiye, Ankara, Turkey.
- 3Department of General Surgery, Antalya University School of Medicine, Dumlupinar Street, 07058, Antalya, Turkey.
- KMID: 1711456
- DOI: http://doi.org/10.3348/kjr.2013.14.6.905
Abstract
- Though congenital anomalies of the pancreas and pancreatic duct are relatively uncommon and they are often discovered as an incidental finding in asymptomatic patients, some of these anomalies may lead to various clinical symptoms such as recurrent abdominal pain, nausea and vomiting. Recognition of these anomalies is important because these anomalies may be a surgically correctable cause of recurrent pancreatitis or the cause of gastric outlet obstruction. An awareness of these anomalies may help in surgical planning and prevent inadvertent ductal injury. The purpose of this article is to review normal pancreatic embryology, the appearance of ductal anatomic variants and developmental anomalies of the pancreas, with emphasis on magnetic resonance cholangiopancreaticography and multidetector computed tomography.
MeSH Terms
Figure
Cited by 2 articles
-
A rare case of choledochal cyst with pancreas divisum: case presentation and literature review
Adrián Ransom-Rodríguez, Ruben Blachman-Braun, Emilio Sánchez-García Ramos, Jesús Varela-Prieto, Erick Rosas-Lezama, Miguel Ángel Mercado
Ann Hepatobiliary Pancreat Surg. 2017;21(1):52-56. doi: 10.14701/ahbps.2017.21.1.52.Exploring the variations of the pancreatic ductal system: a systematic review and meta-analysis of observational studies
Adil Asghar, Ravi Kant Narayan, Nagavalli Basavanna Pushpa, Apurba Patra, Kumar Satish Ravi, R. Shane Tubbs
Anat Cell Biol. 2024;57(1):31-44. doi: 10.5115/acb.23.148.
Reference
-
1. Itoh S, Ikeda M, Ota T, Satake H, Takai K, Ishigaki T. Assessment of the pancreatic and intrapancreatic bile ducts using 0.5-mm collimation and multiplanar reformatted images in multislice CT. Eur Radiol. 2003; 13:277–285.2. Itoh S, Fukushima H, Takada A, Suzuki K, Satake H, Ishigaki T. Assessment of anomalous pancreaticobiliary ductal junction with high-resolution multiplanar reformatted images in MDCT. AJR Am J Roentgenol. 2006; 187:668–675.3. Schulte SJ. Embryology, normal variation, and congenital anomalies of the pancreas. In : Stevenson GW, Freeny PC, Margulis AR, Burhenne HJ, editors. Margulis' and Burhenne's alimentary tract radiology. 5th ed. St. Louis: Mosby;1994. p. 1039–1051.4. Mortelé KJ, Rocha TC, Streeter JL, Taylor AJ. Multimodality imaging of pancreatic and biliary congenital anomalies. Radiographics. 2006; 26:715–731.5. Cha SW, Park MS, Kim KW, Byun JH, Yu JS, Kim MJ, et al. Choledochal cyst and anomalous pancreaticobiliary ductal union in adults: radiological spectrum and complications. J Comput Assist Tomogr. 2008; 32:17–22.6. Kozu T, Suda K, Toki F. Pancreatic development and anatomical variation. Gastrointest Endosc Clin N Am. 1995; 5:1–30.7. Quest L, Lombard M. Pancreas divisum: opinio divisa. Gut. 2000; 47:317–319.8. Soto JA, Lucey BC, Stuhlfaut JW. Pancreas divisum: depiction with multi-detector row CT. Radiology. 2005; 235:503–508.9. Sandrasegaran K, Patel A, Fogel EL, Zyromski NJ, Pitt HA. Annular pancreas in adults. AJR Am J Roentgenol. 2009; 193:455–460.10. Rizzo RJ, Szucs RA, Turner MA. Congenital abnormalities of the pancreas and biliary tree in adults. Radiographics. 1995; 15:49–68. quiz 147-148.11. Nijs EL, Callahan MJ. Congenital and developmental pancreatic anomalies: ultrasound, computed tomography, and magnetic resonance imaging features. Semin Ultrasound CT MR. 2007; 28:395–401.12. Yu J, Turner MA, Fulcher AS, Halvorsen RA. Congenital anomalies and normal variants of the pancreaticobiliary tract and the pancreas in adults: part 2, Pancreatic duct and pancreas. AJR Am J Roentgenol. 2006; 187:1544–1553.13. Emerson L, Layfield LJ, Rohr LR, Dayton MT. Adenocarcinoma arising in association with gastric heterotopic pancreas: a case report and review of the literature. J Surg Oncol. 2004; 87:53–57.14. Alexander LF. Congenital pancreatic anomalies, variants, and conditions. Radiol Clin North Am. 2012; 50:487–498.15. Low JP, Williams D, Chaganti JR. Polysplenia syndrome with agenesis of the dorsal pancreas and preduodenal portal vein presenting with obstructive jaundice--a case report and literature review. Br J Radiol. 2011; 84:e217–e220.16. Lång K, Lasson A, Müller MF, Thorlacius H, Toth E, Olsson R. Dorsal agenesis of the pancreas - a rare cause of abdominal pain and insulin-dependent diabetes. Acta Radiol. 2012; 53:2–4.17. Oeda S, Otsuka T, Akiyama T, Ario K, Masuda M, Taguchi S, et al. Recurrent acute pancreatitis caused by a gastric duplication cyst communicating with an aberrant pancreatic duct. Intern Med. 2010; 49:1371–1375.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pancreas Neuroendocrine Tumor and Its Mimics: Review of Cross-Sectional Imaging Findings for Differential Diagnosis
- Preoperative Radiologic Evaluation of Cholangiocarcinoma
- Imaging Findings of Primary Angiomyolipoma of the Pancreas: A Case Report
- Squamous Cell Carcinoma of the Pancreas: A Case Report
- Aortic Arch Variants and Anomalies: Embryology, Imaging Findings, and Clinical Considerations