Korean J Radiol.
2014 Apr;15(2):267-276. 10.3348/kjr.2014.15.2.267.
Thyroid Ultrasonography: Pitfalls and Techniques
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul 120-752, Korea. docjin@yuhs.ac
- 2Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul 110-746, Korea.
- 3Department of Radiology, Chung-Ang University Hospital, Seoul 156-755, Korea.
- KMID: 1705583
- DOI: http://doi.org/10.3348/kjr.2014.15.2.267
Abstract
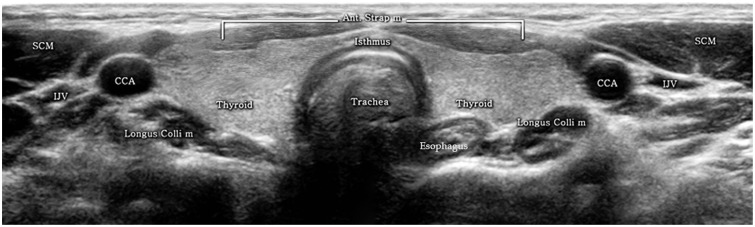
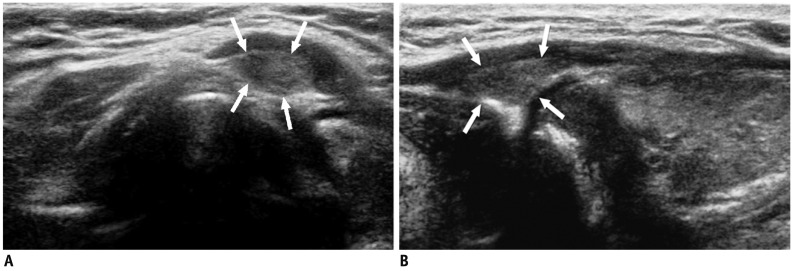
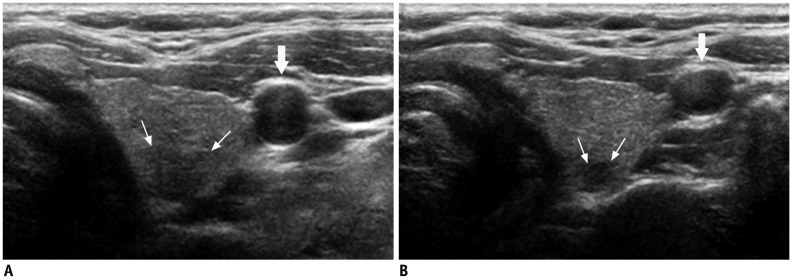
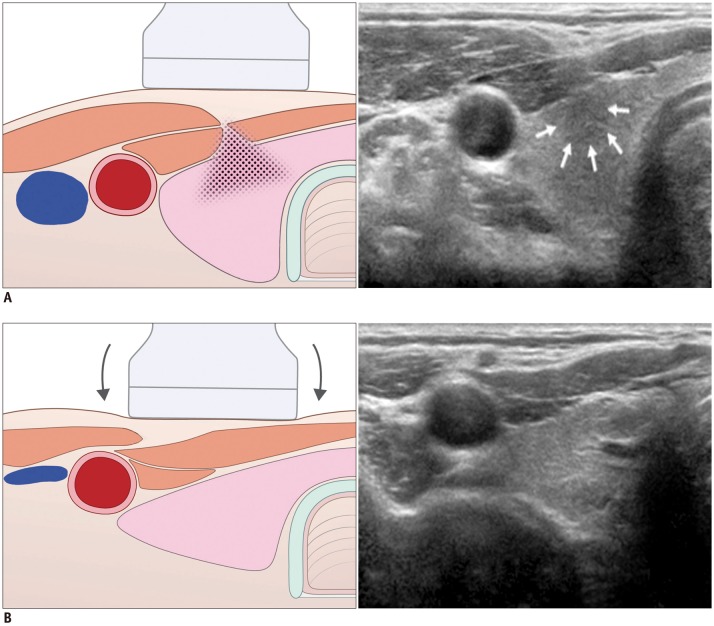
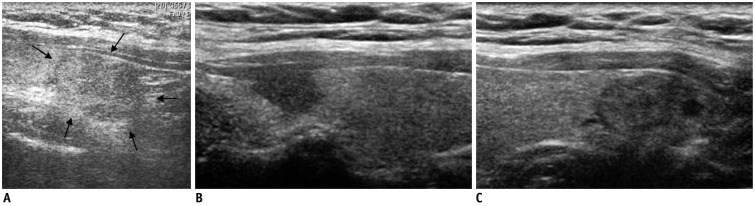
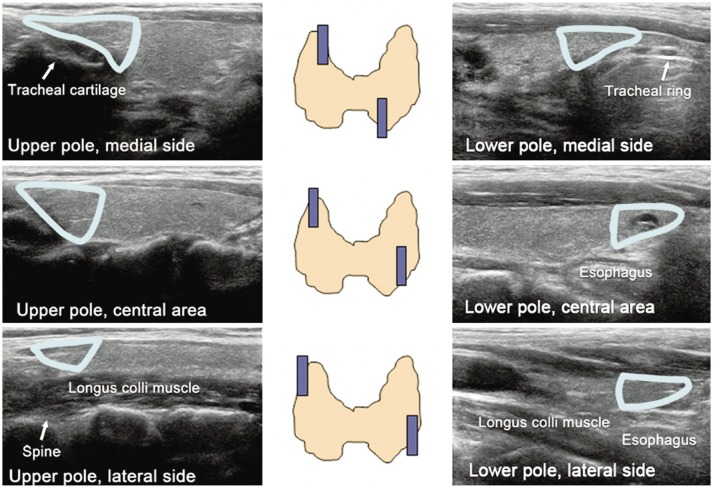
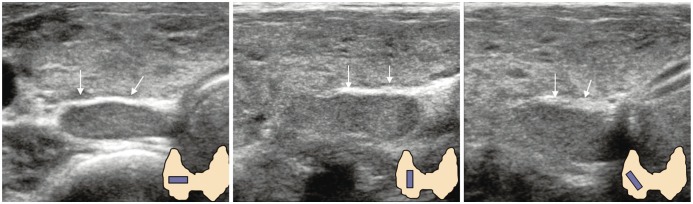
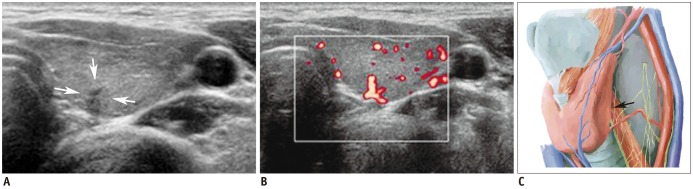
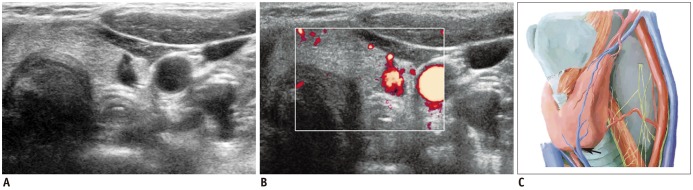
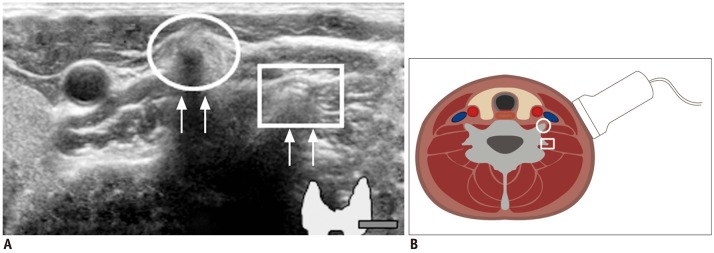
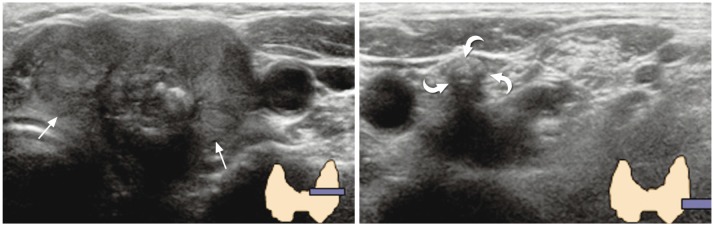
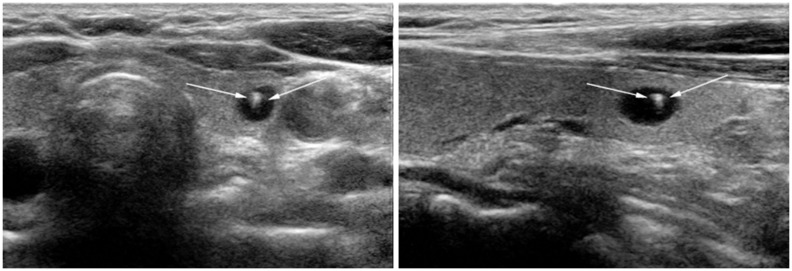
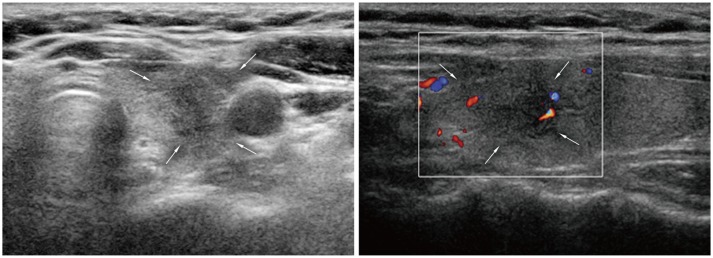
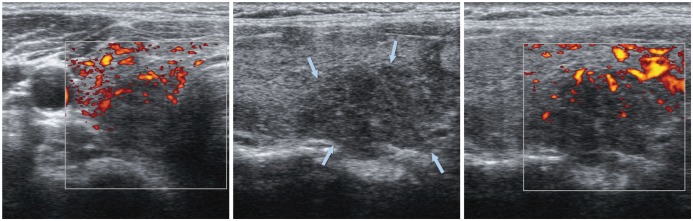
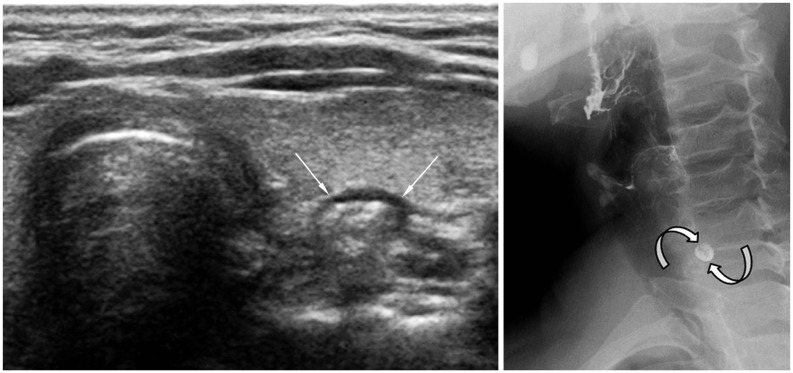
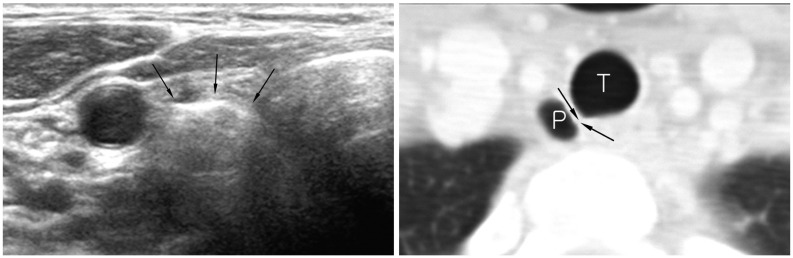
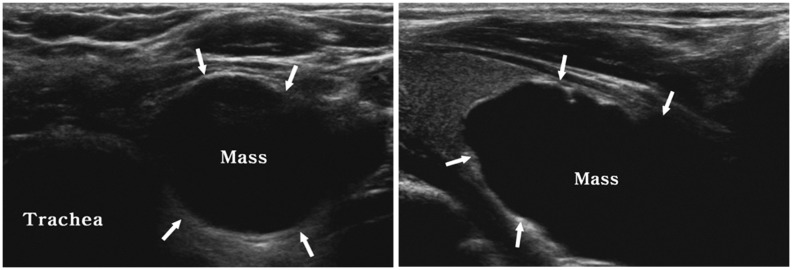
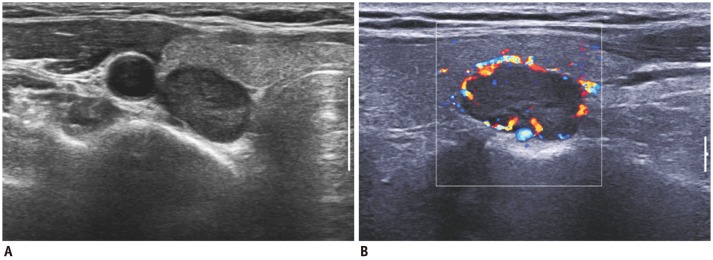
- Thyroid ultrasonography (US) plays a key role in the diagnosis and management of thyroid-related diseases. The aim of this article was to illustrate various pitfalls that can occur in utilizing thyroid US and techniques to prevent them. In this article, we present cases demonstrating the common pitfalls associated with US equipment, performance, normal thyroid structures, misinterpretations, and surrounding structures. Knowledge of these areas is essential to avoid misdiagnosis or improper disease management.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Radiofrequency versus Ethanol Ablation for Treating Predominantly Cystic Thyroid Nodules: A Randomized Clinical Trial
Jung Hwan Baek, Eun Ju Ha, Young Jun Choi, Jin Yong Sung, Jae Kyun Kim, Young Kee Shong
Korean J Radiol. 2015;16(6):1332-1340. doi: 10.3348/kjr.2015.16.6.1332.2019 Practice guidelines for thyroid core needle biopsy: a report of the Clinical Practice Guidelines Development Committee of the Korean Thyroid Association
Chan Kwon Jung, Jung Hwan Baek, Dong Gyu Na, Young Lyun Oh, Ka Hee Yi, Ho-Cheol Kang
J Pathol Transl Med. 2020;54(1):64-86. doi: 10.4132/jptm.2019.12.04.
Reference
-
1. Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002; 178:687–691. PMID: 11856699.
Article2. Mazzaferri EL. Management of a solitary thyroid nodule. N Engl J Med. 1993; 328:553–559. PMID: 8426623.
Article3. Rosen IB, Azadian A, Walfish PG, Salem S, Lansdown E, Bedard YC. Ultrasound-guided fine-needle aspiration biopsy in the management of thyroid disease. Am J Surg. 1993; 166:346–349. PMID: 8214289.
Article4. Yokozawa T, Miyauchi A, Kuma K, Sugawara M. Accurate and simple method of diagnosing thyroid nodules the modified technique of ultrasound-guided fine needle aspiration biopsy. Thyroid. 1995; 5:141–145. PMID: 7647575.5. Koike E, Yamashita H, Noguchi S, Murakami T, Ohshima A, Maruta J, et al. Effect of combining ultrasonography and ultrasound-guided fine-needle aspiration biopsy findings for the diagnosis of thyroid nodules. Eur J Surg. 2001; 167:656–661. PMID: 11759733.6. Peccin S, de Castsro JA, Furlanetto TW, Furtado AP, Brasil BA, Czepielewski MA. Ultrasonography: is it useful in the diagnosis of cancer in thyroid nodules? J Endocrinol Invest. 2002; 25:39–43. PMID: 11885575.
Article7. Butch RJ, Simeone JF, Mueller PR. Thyroid and parathyroid ultrasonography. Radiol Clin North Am. 1985; 23:57–71. PMID: 3883407.8. Khati N, Adamson T, Johnson KS, Hill MC. Ultrasound of the thyroid and parathyroid glands. Ultrasound Q. 2003; 19:162–176. PMID: 14730259.
Article9. Barraclough BM, Barraclough BH. Ultrasound of the thyroid and parathyroid glands. World J Surg. 2000; 24:158–165. PMID: 10633142.
Article10. Slapa RZ, Slowinska-Srzednicka J, Szopinski KT, Jakubowski W. Gray-scale three-dimensional sonography of thyroid nodules: feasibility of the method and preliminary studies. Eur Radiol. 2006; 16:428–436. PMID: 16155720.
Article11. Hoang JK, Lee WK, Lee M, Johnson D, Farrell S. US Features of thyroid malignancy: pearls and pitfalls. Radiographics. 2007; 27:847–860. discussion 861-865. PMID: 17495296.
Article12. Kwak JY, Kim EK, Park SY, Kim MJ, Moon WJ, Choi SH, et al. Findings of extrathyroid lesions encountered with thyroid sonography. J Ultrasound Med. 2007; 26:1747–1759. PMID: 18029927.
Article13. Macdonald AJ. Diagnostic and surgical imaging anatomy. Brain, head & neck, spine. Salt Lake City: Amirsys;2006. p. II-230.14. Gritzmann N, Koischwitz D, Rettenbacher T. Sonography of the thyroid and parathyroid glands. Radiol Clin North Am. 2000; 38:1131–1145. xiiPMID: 11054973.
Article15. Desser TS, Kamaya A. Ultrasound of thyroid nodules. Neuroimaging Clin N Am. 2008; 18:463–478. viiPMID: 18656028.
Article16. Kamaya A, Quon A, Jeffrey RB. Sonography of the abnormal parathyroid gland. Ultrasound Q. 2006; 22:253–262. PMID: 17146333.
Article17. Nilsson A. Artefacts in sonography and Doppler. Eur Radiol. 2001; 11:1308–1315. PMID: 11519537.
Article18. Rumack CM, Wilson SR, Charboneau JW, Levine D. Diagnostic ultrasound. 4th ed. Philadelphia: Elsevier Mosby;2011. p. 20–21. p. 798–800.19. Stavros AT. Breast ultrasound. Philadelphia: Lippincott Williams & Wilkins;2004. p. 488–494.20. Berbaum KS, Franken EA Jr, Dorfman DD, Rooholamini SA, Kathol MH, Barloon TJ, et al. Satisfaction of search in diagnostic radiology. Invest Radiol. 1990; 25:133–140. PMID: 2312249.
Article21. Langer JE, Mandel SJ. Sonographic imaging of cervical lymph nodes in patients with thyroid cancer. Neuroimaging Clin N Am. 2008; 18:479–489. vii–viii. PMID: 18656029.
Article22. Leboulleux S, Girard E, Rose M, Travagli JP, Sabbah N, Caillou B, et al. Ultrasound criteria of malignancy for cervical lymph nodes in patients followed up for differentiated thyroid cancer. J Clin Endocrinol Metab. 2007; 92:3590–3594. PMID: 17609301.
Article23. Kuna SK, Bracic I, Tesic V, Kuna K, Herceg GH, Dodig D. Ultrasonographic differentiation of benign from malignant neck lymphadenopathy in thyroid cancer. J Ultrasound Med. 2006; 25:1531–1537. quiz 1538-1540. PMID: 17121947.
Article24. Stanley MW, Knoedler JP. Skeletal structures that clinically simulate lymph nodes: encounters during fine-needle aspiration. Diagn Cytopathol. 1993; 9:86–88. PMID: 8458291.
Article25. Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002; 87:1941–1946. PMID: 11994321.
Article26. Cappelli C, Castellano M, Pirola I, Cumetti D, Agosti B, Gandossi E, et al. The predictive value of ultrasound findings in the management of thyroid nodules. QJM. 2007; 100:29–35. PMID: 17178736.
Article27. Ito Y, Kobayashi K, Tomoda C, Uruno T, Takamura Y, Miya A, et al. Ill-defined edge on ultrasonographic examination can be a marker of aggressive characteristic of papillary thyroid microcarcinoma. World J Surg. 2005; 29:1007–1011. discussion 1011-1012. PMID: 15981041.
Article28. Cappelli C, Castellano M, Pirola I, Gandossi E, De Martino E, Cumetti D, et al. Thyroid nodule shape suggests malignancy. Eur J Endocrinol. 2006; 155:27–31. PMID: 16793946.
Article29. Moon WJ, Baek JH, Jung SL, Kim DW, Kim EK, Kim JY, et al. Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J Radiol. 2011; 12:1–14. PMID: 21228935.
Article30. Khoo ML, Asa SL, Witterick IJ, Freeman JL. Thyroid calcification and its association with thyroid carcinoma. Head Neck. 2002; 24:651–655. PMID: 12112538.
Article31. Ahuja A, Chick W, King W, Metreweli C. Clinical significance of the comet-tail artifact in thyroid ultrasound. J Clin Ultrasound. 1996; 24:129–133. PMID: 8838301.
Article32. Park SY, Kim EK, Kim MJ, Kim BM, Oh KK, Hong SW, et al. Ultrasonographic characteristics of subacute granulomatous thyroiditis. Korean J Radiol. 2006; 7:229–234. PMID: 17143025.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound elastography for thyroid nodules: recent advances
- Ultrasound elastography of the thyroid: principles and current status
- Effective and Safe Application of Radiofrequency Ablation for Benign Thyroid Nodules
- Ultrasonography of pediatric urogenital emergencies: review of classic and new techniques
- Sonographic Evaluation of Thyroid Nodules