Korean J Radiol.
2014 Apr;15(2):245-249. 10.3348/kjr.2014.15.2.245.
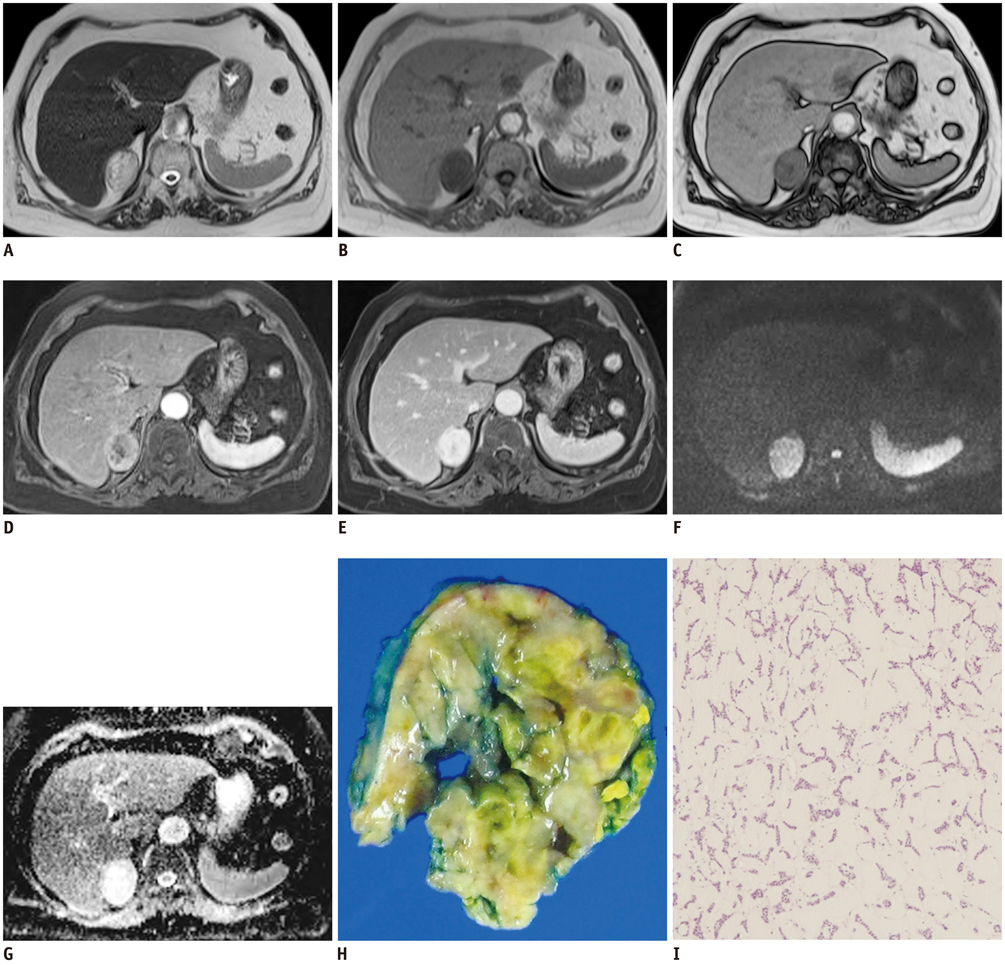
Myxoid Adrenocortical Adenoma: Magnetic Resonance Imaging and Pathology Correlation
- Affiliations
-
- 1Department of Radiology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan 626-770, Korea.
- 2Department of Radiology, Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan 602-739, Korea. kimsuk@medimail.co.kr
- 3Department of Urology, Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan 602-739, Korea.
- 4Department of Pathology, Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan 602-739, Korea.
- KMID: 1705579
- DOI: http://doi.org/10.3348/kjr.2014.15.2.245
Abstract
- We report a case of a 74-year-old female with myxoid adrenocortical adenoma which showed different magnetic resonance imaging findings compared to those of a typical adrenocortical adenoma. The myxoid change in the adrenocortical adenoma is a rare form of degeneration. It presents a considerable diagnostic challenge to both radiologists and clinicians because it can mimic other adrenal tumor types on imaging. The MRI findings of the presented case included a high signal intensity on T2-weighted images similar to that of fluid and delayed progressive enhancement.
Keyword
MeSH Terms
Figure
Reference
-
1. Peña CS, Boland GW, Hahn PF, Lee MJ, Mueller PR. Characterization of indeterminate (lipid-poor) adrenal masses: use of washout characteristics at contrast-enhanced CT. Radiology. 2000; 217:798–802.2. Haider MA, Ghai S, Jhaveri K, Lockwood G. Chemical shift MR imaging of hyperattenuating (>10 HU) adrenal masses: does it still have a role? Radiology. 2004; 231:711–716.3. Tang CK, Harriman BB, Toker C. Myxoid adrenal cortical carcinoma: a light and electron microscopic study. Arch Pathol Lab Med. 1979; 103:635–638.4. Allen PW. Myxoma is not a single entity: a review of the concept of myxoma. Ann Diagn Pathol. 2000; 4:99–123.5. Forsthoefel KF. Myxoid adrenal cortical carcinoma. A case report with differential diagnostic considerations. Arch Pathol Lab Med. 1994; 118:1151–1153.6. Brown FM, Gaffey TA, Wold LE, Lloyd RV. Myxoid neoplasms of the adrenal cortex: a rare histologic variant. Am J Surg Pathol. 2000; 24:396–401.7. Honda K, Kashima K, Daa T, Gamachi A, Nakayama I, Yokoyama S. Myxoid adrenal cortical adenoma. Pathol Int. 2001; 51:887–891.8. Dundr P, Novák K. Pseudoglandular myxoid adenoma of the adrenal gland. Pathol Res Pract. 2003; 199:493–496.9. Bollito ER, Papotti M, Porpiglia F, Terzolo M, Cracco CM, Cappia S, et al. Myxoid adrenocortical adenoma with a pseudoglandular pattern. Virchows Arch. 2004; 445:414–418.10. Wu JS, Hochman MG. Soft-tissue tumors and tumorlike lesions: a systematic imaging approach. Radiology. 2009; 253:297–316.11. Bydder GM. Clinical application of gadolinium-DTPA. In : Stark DD, Bradley WG, editors. Magnetic resonance imaging. St. Louis: Mosby;1988. p. 182–200.12. Mitchell DG, Crovello M, Matteucci T, Petersen RO, Miettinen MM. Benign adrenocortical masses: diagnosis with chemical shift MR imaging. Radiology. 1992; 185:345–351.13. Varghese JC, Hahn PF, Papanicolaou N, Mayo-Smith WW, Gaa JA, Lee MJ. MR differentiation of phaeochromocytoma from other adrenal lesions based on qualitative analysis of T2 relaxation times. Clin Radiol. 1997; 52:603–606.14. Inan N, Arslan A, Akansel G, Anik Y, Balci NC, Demirci A. Dynamic contrast enhanced MRI in the differential diagnosis of adrenal adenomas and malignant adrenal masses. Eur J Radiol. 2008; 65:154–162.15. Sakai F, Sone S, Kiyono K, Maruyama A, Ueda H, Aoki J, et al. Intrathoracic neurogenic tumors: MR-pathologic correlation. AJR Am J Roentgenol. 1992; 159:279–283.16. Dunnick NR, Castellino RA. Arteriographic Manifestations of Ganglioneuromas. Radiology. 1975; 115:323–328.17. Ichikawa T, Ohtomo K, Araki T, Fujimoto H, Nemoto K, Nanbu A, et al. Ganglioneuroma: computed tomography and magnetic resonance features. Br J Radiol. 1996; 69:114–121.18. Liu QY, Gao M, Li HG, Lin XF, Huang SQ, Liang BL. Juxta-adrenal schwannoma: dynamic multi-slice CT and MRI findings. Eur J Radiol. 2012; 81:794–799.19. Suzuki K, Nakanishi A, Kurosaki Y, Nogaki J, Takaba E. Adrenal schwannoma: CT and MRI findings. Radiat Med. 2007; 25:299–302.20. Takatera H, Takiuchi H, Namiki M, Takaha M, Ohnishi S, Sonoda T. Retroperitoneal schwannoma. Urology. 1986; 28:529–531.21. Sabanegh E Jr, Harris MJ, Grider D. Cavernous adrenal hemangioma. Urology. 1993; 42:327–330.22. Otal P, Escourrou G, Mazerolles C, Janne d'Othee B, Mezghani S, Musso S, et al. Imaging features of uncommon adrenal masses with histopathologic correlation. Radiographics. 1999; 19:569–581.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Computed Tomography and Magnetic Resonance Images of Adrenocortical Oncocytoma Cases
- The Magnetic Resonance (MR) Imaging Features of Myxoid Liposarcoma Arising from the Mesentery: a Case Report
- Cushing syndrome in pregnancy secondary to adrenal adenoma
- A case of virilizing adrenocortical adenoma
- Identification of Fat in Myxoid Matrix-Rich Mesenteric Lipoblastoma Using In-Phase and Opposed-Phase MRI: A Case Report