Clin Orthop Surg.
2013 Sep;5(3):174-179. 10.4055/cios.2013.5.3.174.
Ceramic-on-Ceramic Total Hip Arthroplasty: Minimum of Six-Year Follow-up Study
- Affiliations
-
- 1Department of Orthopaedic Surgery, Eulji University Hospital, Eulji University School of Medicine, Daejeon, Korea. oskkj@eulji.ac.kr
- KMID: 1705542
- DOI: http://doi.org/10.4055/cios.2013.5.3.174
Abstract
- BACKGROUND
This study examines the clinical and radiologic results of ceramic-on-ceramic total hip arthroplasties with regard to wear, osteolysis, and fracture of the ceramic after a minimum follow-up of six years.
METHODS
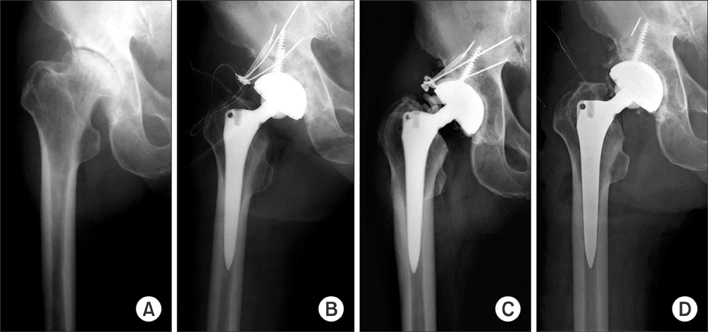
We evaluated the results of a consecutive series of 148 primary ceramic-on-ceramic total hip arthroplasties that had been performed between May 2001 and October 2005 in 142 patients. The mean age was 57.2 years (range, 23 to 81 years). The mean follow-up period was 7.8 years (range, 6.1 to 10.1 years). Preoperative diagnosis was avascular necrosis in 77 hips (52%), degenerative arthritis in 36 hips (24.3%), femur neck fracture in 18 hips (12.2%), rheumatoid arthritis in 15 hips (10.1%), and septic hip sequelae in 2 hips (1.4%). Clinical results were evaluated with the Harris hip score, and the presence of postoperative groin or thigh pain. Radiologic analysis was done with special attention in terms of wear, periprosthetic osteolysis, and ceramic failures.
RESULTS
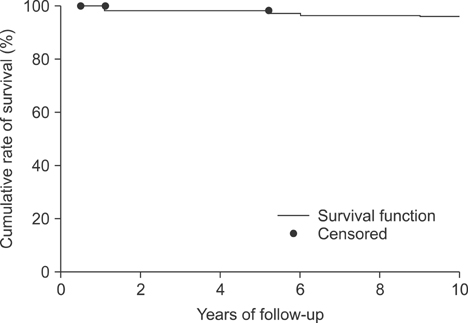
The mean Harris hip score improved from 58.3 (range, 10 to 73) to 92.5 (range, 79 to 100) on the latest follow-up evaluation. At final follow-up, groin pain was found in 4 hips (2.7%), and thigh pain was found in 6 hips (4.1%). Radiologically, all femoral stems demonstrated stable fixations without loosening. Radiolucent lines were observed around the stem in 25 hips (16.9%), and around the cup in 4 hips (2.7%). Endosteal new bone formation was observed around the stem in 95 hips (64.2%) and around the cup in 88 hips (59.5%). No osteolysis was observed around the stem and cup. There were 2 hips (1.4%) of inclination changes of acetabular cup, 2 hips (1.4%) of hip dislocation, 1 hip (0.7%) of ceramic head fracture, and 1 hip (0.7%) of squeaking. The Kaplan-Meier survival rate of the prostheses was 98.1% at postoperative 7.8 years.
CONCLUSIONS
The ceramic-on-ceramic total hip arthroplasty produced excellent clinical results and implant survival rates with no detectable osteolysis on a minimum six-year follow-up study. The ceramic-on-ceramic couplings could be a reasonable option of primary total hip arthroplasty for variable indications.
Keyword
MeSH Terms
Figure
Reference
-
1. Maloney WJ, Jasty M, Harris WH, Galante JO, Callaghan JJ. Endosteal erosion in association with stable uncemented femoral components. J Bone Joint Surg Am. 1990; 72(7):1025–1034.
Article2. Schmalzried TP, Jasty M, Harris WH. Periprosthetic bone loss in total hip arthroplasty: polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg Am. 1992; 74(6):849–863.
Article3. Sedel L. Evolution of alumina-on-alumina implants: a review. Clin Orthop Relat Res. 2000; (379):48–54.4. Yoo JJ, Kim YM, Yoon KS, Koo KH, Song WS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a five-year minimum follow-up study. J Bone Joint Surg Am. 2005; 87(3):530–535.5. Lee YK, Ha YC, Yoo JJ, Koo KH, Yoon KS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a concise follow-up, at a minimum of ten years, of a previous report. J Bone Joint Surg Am. 2010; 92(8):1715–1719.6. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51(4):737–755.
Article7. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.
Article8. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.9. Olyslaegers C, Defoort K, Simon JP, Vandenberghe L. Wear in conventional and highly cross-linked polyethylene cups: a 5-year follow-up study. J Arthroplasty. 2008; 23(4):489–494.10. Shia DS, Clohisy JC, Schinsky MF, Martell JM, Maloney WJ. THA with highly cross-linked polyethylene in patients 50 years or younger. Clin Orthop Relat Res. 2009; 467(8):2059–2065.
Article11. Calvert GT, Devane PA, Fielden J, Adams K, Horne JG. A double-blind, prospective, randomized controlled trial comparing highly cross-linked and conventional polyethylene in primary total hip arthroplasty. J Arthroplasty. 2009; 24(4):505–510.
Article12. Langkamer VG, Case CP, Collins C, et al. Tumors around implants. J Arthroplasty. 1997; 12(7):812–818.
Article13. Bierbaum BE, Nairus J, Kuesis D, Morrison JC, Ward D. Ceramic-on-ceramic bearings in total hip arthroplasty. Clin Orthop Relat Res. 2002; (405):158–163.
Article14. Saikko VO, Paavolainen PO, Slatis P. Wear of the polyethylene acetabular cup: metallic and ceramic heads compared in a hip simulator. Acta Orthop Scand. 1993; 64(4):391–402.
Article15. D'Antonio JA, Capello WN, Naughton M. Ceramic bearings for total hip arthroplasty have high survivorship at 10 years. Clin Orthop Relat Res. 2012; 470(2):373–381.16. Willmann G. Ceramic femoral head retrieval data. Clin Orthop Relat Res. 2000; (379):22–28.
Article17. Hasegawa M, Sudo A, Hirata H, Uchida A. Ceramic acetabular liner fracture in total hip arthroplasty with a ceramic sandwich cup. J Arthroplasty. 2003; 18(5):658–661.
Article18. Koo KH, Ha YC, Jung WH, Kim SR, Yoo JJ, Kim HJ. Isolated fracture of the ceramic head after third-generation alumina-on-alumina total hip arthroplasty. J Bone Joint Surg Am. 2008; 90(2):329–336.
Article19. Keurentjes JC, Kuipers RM, Wever DJ, Schreurs BW. High incidence of squeaking in THAs with alumina ceramic-on-ceramic bearings. Clin Orthop Relat Res. 2008; 466(6):1438–1443.
Article20. Lusty PJ, Tai CC, Sew-Hoy RP, Walter WL, Walter WK, Zicat BA. Third-generation alumina-on-alumina ceramic bearings in cementless total hip arthroplasty. J Bone Joint Surg Am. 2007; 89(12):2676–2683.
Article21. Chevillotte C, Trousdale RT, Chen Q, Guyen O, An KN. The 2009 Frank Stinchfield Award: "Hip squeaking": a biomechanical study of ceramic-on-ceramic bearing surfaces. Clin Orthop Relat Res. 2010; 468(2):345–350.22. Baek SH, Kim SY. Cementless total hip arthroplasty with alumina bearings in patients younger than fifty with femoral head osteonecrosis. J Bone Joint Surg Am. 2008; 90(6):1314–1320.
Article23. Mai K, Verioti C, Ezzet KA, Copp SN, Walker RH, Colwell CW Jr. Incidence of 'squeaking' after ceramic-on-ceramic total hip arthroplasty. Clin Orthop Relat Res. 2010; 468(2):413–417.
Article24. Morlock M, Nassutt R, Janssen R, Willmann G, Honl M. Mismatched wear couple zirconium oxide and aluminum oxide in total hip arthroplasty. J Arthroplasty. 2001; 16(8):1071–1074.
Article25. Walter WL, O'toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty. 2007; 22(4):496–503.26. Taylor S, Manley MT, Sutton K. The role of stripe wear in causing acoustic emissions from alumina ceramic-on-ceramic bearings. J Arthroplasty. 2007; 22:7 Suppl 3. 47–51.
Article27. McCollum DE, Gray WJ. Dislocation after total hip arthroplasty: causes and prevention. Clin Orthop Relat Res. 1990; (261):159–170.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ceramic Head Fracture in Ceramic-on-Polyethylene Total Hip Arthroplasty
- Early Comminuted Fracture of an Alumina Liner in a Ceramic on Ceramic Total Hip Arthroplasty
- Short-term Results of Cementless Ceramic-on-ceramic Articulation Total Hip Arthroplasty
- A Case of Failure of a Ceramic Head in Total Hip Arthroplasty: A Case Report
- Non-traumatic Ceramic Head Fracture in Total Hip Arthroplasty with Ceramic-on-Ceramic Articulation at Postoperative 16th Years