J Korean Soc Endocrinol.
2006 Apr;21(2):132-141. 10.3803/jkes.2006.21.2.132.
Clinical Characteristics of Poorly Differentiated Carcinoma of the Thyroid and Comparison of Its Survival to the Tall Cell and Columnar Cell Variants of Papillary Carcinoma
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea.
- 2Department of Medicine and Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea.
- 3Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Korea.
- 4Department of Internal Medicine, Seoul National University College of Medicine, Korea.
- KMID: 1511952
- DOI: http://doi.org/10.3803/jkes.2006.21.2.132
Abstract
-
BACKGROUND: Poorly differentiated carcinoma (PDC) of the thyroid includes tall and columnar cell variants (TCV) of the papillary carcinoma as well as the thyroid carcinoma with trabecular, insular and solid (TIS) growth patterns. There have been a few clinical studies on the PDC of the thyroid. We evaluated the clinical characteristics and the outcome of the PDC.
METHODS
We investigated the clinicopathologic features of the thyroid carcinoma with TIS growth patterns (n = 46) and TCV of the papillary carcinoma (n = 14). We investigated the clinical features of ten patients diagnosed as PDC of the thyroid who had been undergone thyroidectomy for well differentiated carcinoma previously and compared these outcome with those of patients primarily diagnosed as PDC of the thyroid (n = 60).
RESULTS
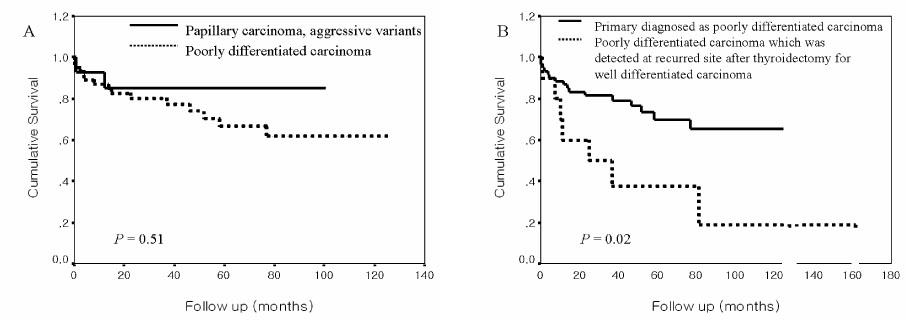
The clinical course of the thyroid carcinoma with TIS growth patterns was slightly more aggressive than that of TCV of the papillary carcinoma. However, disease-specific survivals of both cancers were not significantly different. Disease-specific survival was independently correlated with the presence of distant metastasis at diagnosis and high dose radioiodine therapy. The clinical features and outcome of the patients with PDC detected at recurred sites after operation for well-differentiated carcinoma were more aggressive than those diagnosed as PDC of the thyroid.
CONCLUSION
The prognosis of the thyroid carcinoma with TIS growth patterns and TCV of the papillary carcinoma were similar. The PDC which was detected after thyroidectomy for well-differentiated carcinoma had worse prognosis than primarily diagnosed as PDC of the thyroid.
MeSH Terms
Figure
Reference
-
1. Carcangiu ML, Zampi G, Rosai J. Poorly differentiated ("insular") thyroid carcinoma. A reinterpretation of Langhans' "wuchernde Struma". Am J Surg Pathol. 1984. 8:655–668.2. Papotti M, Botto Micca F, Favero A, Palestini N, Bussolati G. Poorly differentiated thyroid carcinomas with primordial cell component. A group of aggressive lesions sharing insular, trabecular, and solid patterns. Am J Surg Pathol. 1993. 17:291–301.3. Sakamoto A, Kasai N, Sugano H. Poorly differentiated carcinoma of the thyroid. A clinicopathologic entity for a high-risk group of papillary and follicular carcinomas. Cancer. 1983. 52:1849–1855.4. Pilotti S, Collini P, Manzari A, Marubini E, Rilke F. Poorly differentiated forms of papillary thyroid carcinoma: distinctive entities or morphological patterns? Semin Diagn Pathol. 1995. 12:249–255.5. Rosai J, Saxen EA, Woolner L. Undifferentiated and poorly differentiated carcinoma. Semin Diagn Pathol. 1985. 2:123–136.6. AJCC cancer staging manual. 2002. 6th ed. New York: Springer-Verlag Press;77–79.7. Pilotti S, Collini P, Mariani L, Placucci M, Bongarzone I, Vigneri P, Cipriani S, Falcetta F, Miceli R, Pierotti MA, Rilke F. Insular carcinoma: a distinct de novo entity among follicular carcinomas of the thyroid gland. Am J Surg Pathol. 1997. 21:1466–1473.8. Pellegriti G, Giuffrida D, Scollo C, Vigneri R, Regalbuto C, Squatrito S, Belfiore A. Long-term outcome of patients with insular carcinoma of the thyroid: the insular histotype is an independent predictor of poor prognosis. Cancer. 2002. 95:2076–2085.9. Ashfaq R, Vuitch F, Delgado R, Albores-Saavedra J. Papillary and follicular thyroid carcinomas with an insular component. Cancer. 1994. 73:416–423.10. Chao TC, Lin JD, Chen MF. Insular carcinoma: infrequent subtype of thyroid cancer with aggressive clinical course. World J Surg. 2004. 28:393–396.11. Lam KY, Lo CY, Chan KW, Wan KY. Insular and anaplastic carcinoma of the thyroid: a 45-year comparative study at a single institution and a review of the significance of p53 and p21. Ann Surg. 2000. 231:329–338.12. Sobrinho-Simoes M, Sambade C, Fonseca E, Soares P. Poorly differentiated carcinomas of the thyroid gland: a review of the clinicopathologic features of a series of 28 cases of a heterogeneous, clinically aggressive group of thyroid tumors. Int J Surg Pathol. 2002. 10:123–131.13. Volante M, Landolfi S, Chiusa L, Palestini N, Motta M, Codegone A, Torchio B, Papotti MG. Poorly differentiated carcinomas of the thyroid with trabecular, insular, and solid patterns: a clinicopathologic study of 183 patients. Cancer. 2004. 100:950–957.14. Robbins J, Merino MJ, Boice JD Jr, Ron E, Ain KB, Alexander HR, Norton JA, Reynolds J. Thyroid cancer: a lethal endocrine neoplasm. Ann Intern Med. 1991. 115:133–147.15. Sobrinho-Simoes M, Nesland JM, Johannessen JV. Columnar-cell carcinoma. Another variant of poorly differentiated carcinoma of the thyroid. Am J Clin Pathol. 1988. 89:264–267.16. Nishida T, Katayama S, Tsujimoto M, Nakamura J, Matsuda H. Clinicopathological significance of poorly differentiated thyroid carcinoma. Am J Surg Pathol. 1999. 23:205–211.17. Johnson TL, Lloyd RV, Thompson NW, Beierwaltes WH, Sisson JC. Prognostic implications of the tall cell variant of papillary thyroid carcinoma. Am J Surg Pathol. 1988. 12:22–27.18. Sobrinho-Simoes M, Sambade C, Nesland JM, Johannessen JV. Tall cell papillary carcinoma. Am J Surg Pathol. 1989. 13:79–80.19. Evans HL. Columnar-cell carcinoma of the thyroid. A report of two cases of an aggressive variant of thyroid carcinoma. Am J Clin Pathol. 1986. 85:77–80.20. Braverman LE, Utiger RD. Werner & Ingbar's the thyroid a fundamental and clinical text. 2005. 9th ed. Philadelphia: Lippincott Williams & Wilkins Press;428–449.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Retraction: Clinical Characteristics of Poorly Differentiated Carcinoma of the Thyroid and Comparison of Survival to Tall Cell and Columnar Cell Variants of the Papillary Carcinoma
- Poorly Differentiated Carcinoma of the Thyroid Retrospective Clinical and mMrphologic Evaluation
- Prognostic Significance of the Tall Cell Variant of Papillary Thyroid Carcinoma: Expression of p53, bcl-2 & Leu-M1 proteins
- Fine Needle Aspiration Cytology of Columnar Cell Variant of Papillary Carcinoma of the Thyroid: A Case Report
- Columnar Cell Variant of Papillary Thyroid Carcinoma: Report of 2 Cases