Yonsei Med J.
2013 Mar;54(2):306-314. 10.3349/ymj.2013.54.2.306.
Health-Related Quality of Life and Cognitive Functioning at On- and Off-Treatment Periods in Children Aged between 6-13 Years Old with Brain Tumors: A Prospective Longitudinal Study
- Affiliations
-
- 1Department of Psychiatry, Seoul Metropolitan Eunpyeong Hospital, Seoul, Korea.
- 2Department of Psychiatry, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. yschoung@skku.edu
- 3Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1503890
- DOI: http://doi.org/10.3349/ymj.2013.54.2.306
Abstract
- PURPOSE
Our study aimed to examine the relationship between intelligence and health-related quality of life (HRQOL) in children (6-13 years old) diagnosed as having a brain tumor.
MATERIALS AND METHODS
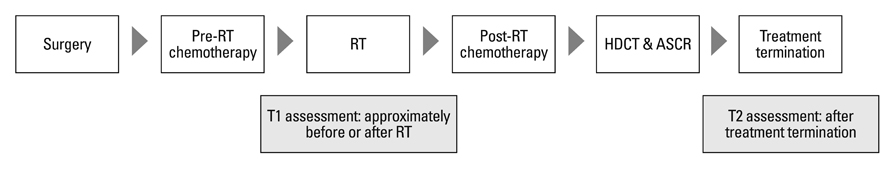
We administered a Korean version of the Wechsler Intelligence Scale for Children-III, the Pediatric Quality of Life Inventory, version 4.0 (PedsQL), the Korean version of the Parenting Stress Index-Short Form, and the Korean Version of the Parenting Sense of Competence (K-PSOC) scale before or after initial radiotherapy (T1) and after treatment termination (T2). In total, 13 patients completed both the T1 and T2 interviews.
RESULTS
Scores significantly declined between T1 and T2 on the full-scale intelligence quotients (FIQ), verbal intelligence quotients (VIQ), performance intelligence quotients (PIQ), similarity and coding tests, as well as the K-PSOC, which measures parental anxiety. FIQ scores at T1 were correlated with the self-reported PedsQL total scores (r=0.739) and the parent proxy-report PedsQL scores for school functioning (r=0.706) at T2. Also, the FIQ scores at T2 were correlated with the self-reported PedsQL total scores (r=0.748) and scores for physical health (r=0.728) at T2.
CONCLUSION
The cognitive ability and intelligence level of the patients significantly declined between on and off treatment periods, and higher intelligence functioning at both on and off treatment was correlated with long-term higher HRQOL. Further investigations that monitor intelligence, HRQOL and parenting stress over a longer period, using a greater number of participants, are needed.
Keyword
MeSH Terms
Figure
Reference
-
1. Steliarova-Foucher E, Stiller C, Kaatsch P, Berrino F, Coebergh JW, Lacour B, et al. Geographical patterns and time trends of cancer incidence and survival among children and adolescents in Europe since the 1970s (the ACCISproject): an epidemiological study. Lancet. 2004. 364:2097–2105.2. Duffner PK. Risk factors for cognitive decline in children treated for brain tumors. Eur J Paediatr Neurol. 2010. 14:106–115.
Article3. Peris-Bonet R, Martínez-García C, Lacour B, Petrovich S, Giner-Ripoll B, Navajas A, et al. Childhood central nervous system tumours--incidence and survival in Europe (1978-1997): report from Automated Childhood Cancer Information System project. Eur J Cancer. 2006. 42:2064–2080.
Article4. Lannering B, Marky I, Lundberg A, Olsson E. Long-term sequelae after pediatric brain tumors: their effect on disability and quality of life. Med Pediatr Oncol. 1990. 18:304–310.
Article5. Mostow EN, Byrne J, Connelly RR, Mulvihill JJ. Quality of life in long-term survivors of CNS tumors of childhood and adolescence. J Clin Oncol. 1991. 9:592–599.
Article6. Zebrack BJ, Gurney JG, Oeffinger K, Whitton J, Packer RJ, Mertens A, et al. Psychological outcomes in long-term survivors of childhood brain cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2004. 22:999–1006.
Article7. Mulhern RK, Butler RW. Neurocognitive sequelae of childhood cancers and their treatment. Pediatr Rehabil. 2004. 7:1–14.8. Zeltzer LK, Recklitis C, Buchbinder D, Zebrack B, Casillas J, Tsao JC, et al. Psychological status in childhood cancer survivors: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2009. 27:2396–2404.
Article9. Fuemmeler BF, Mullins LL, Marx BP. Posttraumatic stress and general distress among parents of children surviving a brain tumor. Child Health Care. 2001. 30:169–182.
Article10. Chien LY, Lo LH, Chen CJ, Chen YC, Chiang CC, Yu Chao YM. Quality of life among primary caregivers of Taiwanese children with brain tumor. Cancer Nurs. 2003. 26:305–311.
Article11. Wijnberg-Williams BJ, Kamps WA, Klip EC, Hoekstra-Weebers JE. Psychological adjustment of parents of pediatric cancer patients revisited: five years later. Psychooncology. 2006. 15:1–8.
Article12. World Health Organization. Constitution of the World Health Organization: Basic Document. 1948. Geneva, Switzerland: World Health Organization.13. Varni JW, Burwinkle TM, Lane MM. Health-related quality of life measurement in pediatric clinical practice: an appraisal and precept for future research and application. Health Qual Life Outcomes. 2005. 3:34.
Article14. Matza LS, Swensen AR, Flood EM, Secnik K, Leidy NK. Assessment of health-related quality of life in children: a review of conceptual, methodological, and regulatory issues. Value Health. 2004. 7:79–92.
Article15. Speechley KN, Barrera M, Shaw AK, Morrison HI, Maunsell E. Health-related quality of life among child and adolescent survivors of childhood cancer. J Clin Oncol. 2006. 24:2536–2543.
Article16. Penn A, Lowis SP, Hunt LP, Shortman RI, Stevens MC, McCarter RL, et al. Health related quality of life in the first year after diagnosis in children with brain tumours compared with matched healthy controls; a prospective longitudinal study. Eur J Cancer. 2008. 44:1243–1252.
Article17. An KJ, Song MS, Sung KW, Joung YS. Health-related quality of life, activities of daily living and parenting stress in children with brain tumors. Psychiatry Investig. 2011. 8:250–255.
Article18. Reimers TS, Mortensen EL, Nysom K, Schmiegelow K. Health-related quality of life in long-term survivors of childhood brain tumors. Pediatr Blood Cancer. 2009. 53:1086–1091.
Article19. Hocking MC, Hobbie WL, Deatrick JA, Lucas MS, Szabo MM, Volpe EM, et al. Neurocognitive and family functioning and quality of life among young adult survivors of childhood brain tumors. Clin Neuropsychol. 2011. 25:942–962.
Article20. Poggi G, Liscio M, Galbiati S, Adduci A, Massimino M, Gandola L, et al. Brain tumors in children and adolescents: cognitive and psychological disorders at different ages. Psychooncology. 2005. 14:386–395.
Article21. Kwak KJ, Park HW, Kim CT. A Study for the Standardization of Korean WISC-3 (1). Korean J Dev Psychol. 2002. 15:19–33.22. Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children's health-related quality of life: an analysis of 13,878 parents' reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007. 5:2.
Article23. Kook SH, Varni JW. Validation of the Korean version of the pediatric quality of life inventory 4.0 (PedsQL) generic core scales in school children and adolescents using the Rasch model. Health Qual Life Outcomes. 2008. 6:41.
Article24. Shin SJ, Chung MJ. Effects of stress, social support and efficacy on mothers' parenting behaviors. Korean J Child Stud. 1998. 19:27–42.25. Park HW, Kwak KJ, Park KB. The development of Korean version of WPPSI: the standardization study (1). Korean J Dev Psychol. 1996. 9:60–70.26. Saury JM, Emanuelson I. Cognitive consequences of the treatment of medulloblastoma among children. Pediatr Neurol. 2011. 44:21–30.
Article27. Spiegler BJ, Bouffet E, Greenberg ML, Rutka JT, Mabbott DJ. Change in neurocognitive functioning after treatment with cranial radiation in childhood. J Clin Oncol. 2004. 22:706–713.
Article28. Schell LM. Culture as a stressor: a revised model of biocultural interaction. Am J Phys Anthropol. 1997. 102:67–77.
Article29. Penn A, Lowis SP, Stevens MC, Hunt LP, Shortman RI, McCarter RJ, et al. Family, demographic and illness-related determinants of HRQL in children with brain tumours in the first year after diagnosis. Pediatr Blood Cancer. 2009. 53:1092–1099.
Article30. Hutchinson KC, Willard VW, Hardy KK, Bonner MJ. Adjustment of caregivers of pediatric patients with brain tumors: a cross-sectional analysis. Psychooncology. 2009. 18:515–523.
Article31. Freeman K, O'Dell C, Meola C. Childhood brain tumors: parental concerns and stressors by phase of illness. J Pediatr Oncol Nurs. 2004. 21:87–97.
Article32. Rabineau KM, Mabe PA, Vega RA. Parenting stress in pediatric oncology populations. J Pediatr Hematol Oncol. 2008. 30:358–365.
Article33. Spinks R, Arndt S, Caspers K, Yucuis R, McKirgan LW, Pfalzgraf C, et al. School achievement strongly predicts midlife IQ. Intelligence. 2007. 35:563–567.
Article34. Hall NM, Kuzminskyte R, Pedersen AD, Ørnbøl E, Fink P. The relationship between cognitive functions, somatization and behavioural coping in patients with multiple functional somatic symptoms. Nord J Psychiatry. 2011. 65:216–224.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Health-Related Quality of Life, Activities of Daily Living and Parenting Stress in Children with Brain Tumors
- Pediatric Quality of Life in Congenital Hypothyroidism: an Indonesian Study
- Associations between Sleep and Work-Related Cognitive and Emotional Functioning in Police Employees
- Identifying Trajectories of Health-related Quality of Life in Mid-life Transition Women: Secondary Data Analysis of Korean Longitudinal Survey of Women & Families
- The Effect of Depression and Cognitive Function on the Geriatric Oral Health Assessment Index in the Elderly