Endocrinol Metab.
2010 Dec;25(4):360-364. 10.3803/EnM.2010.25.4.360.
A Case of Thyroid Amyloidosis Misrecognized as Subacute Thyroiditis
- Affiliations
-
- 1Department of Internal Medicine, Dongguk University College of Medicine, Gyeongju, Korea. ysbae28@medimail.co.kr
- 2Department of Diagnostic Radiology, Dongguk University College of Medicine, Gyeongju, Korea.
- 3Department of Pathology, Dongguk University College of Medicine, Gyeongju, Korea.
- KMID: 1497763
- DOI: http://doi.org/10.3803/EnM.2010.25.4.360
Abstract
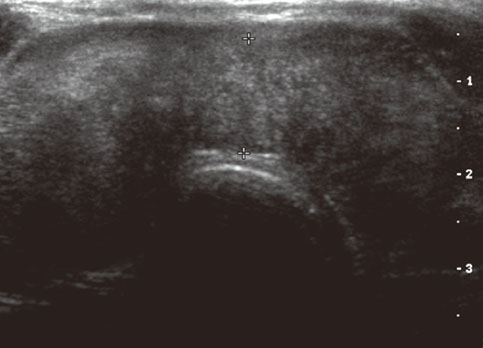
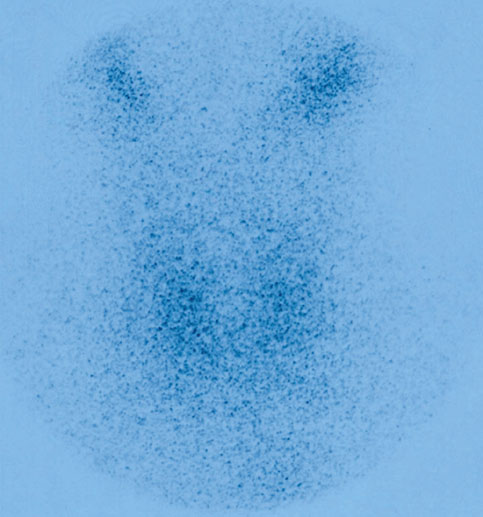
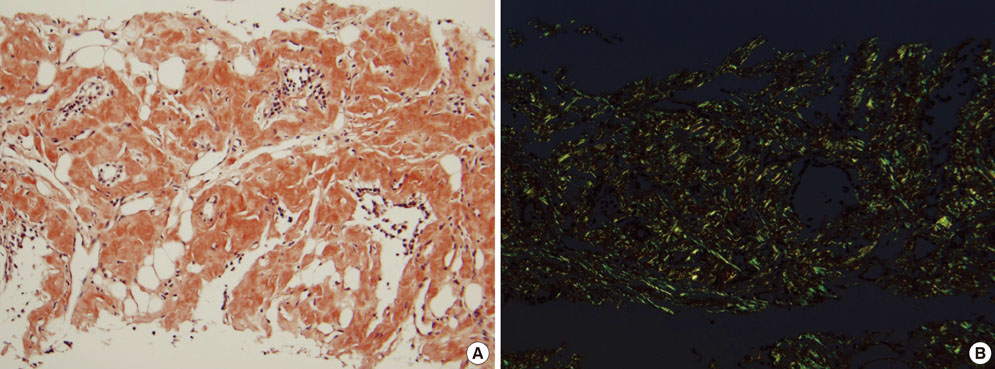
- Amyloid deposition in the thyroid is found in about 30-80% of the patients with primary or secondary amyloidosis. In a few patients with amyloidosis, the thyroid is enlarged and so called amyloid goiter occurs. The thyroid function usually remains normal, but occasionally hypothyroidism or thyrotoxicosis occurs in patients with thyroid amyloidosis. We have experienced one case of thyroid amyloidosis due to bronchiectasis and the patient developed painful goiter and transient thyrotoxicosis resembling subacute thyroiditis. Biopsies from the gastric antrum, duodenum, colon, kidney and thyroid were positive for deposition of amyloid. When patients have signs and symptoms of subacute thyroiditis, but they develop an unusual course, then the diagnosis of thyroid amyloidosis should be considered.
Keyword
MeSH Terms
Figure
Reference
-
1. Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med. 2003. 349:583–596.2. Hirschfield GM. Amyloidosis: a clinico-patho-physiological synopsis. Semin Cell Dev Biol. 2004. 15:39–44.3. Han ST, Kim MS, Yu JM, Yea CJ, Byun JW, Han BG, Choi SO. Secondary amyloidosis in patient with spinal cord injury: renal and thyroid amyloidosis. Korean J Nephrol. 2006. 25:109–113.4. Park CK, Yang YC, Lee CH, Jeong JR, Kim DH, Suh JH, Park JH, Kim YI. A case of secondary amyloid goiter with hypothyroidism. J Korean Soc Endocrinol. 1999. 14:752–756.5. Yildiz L, Kefeli M, Kose B, Baris S. Amyloid goiter: two cases and a review of the literature. Ann Saudi Med. 2009. 29:138–141.6. Yoo YK, Yoon SN, Sohn CI, Kim JH, Kim IS, Ahn YH, Kim MH. Thyroid amyloidosis with subacute thyroiditis-like syndrome. Korean J Med. 1994. 47:574–582.7. Nagai Y, Ohta M, Yokoyama H, Takamura T, Kobayashi KI. Amyloid goiter presented as a subacute thyroiditis-like symptom in a patient with hypersensitivity vasculitis. Endocr J. 1998. 45:421–425.8. Ozdemir BH, Uyar P, Ozdemir FN. Diagnosing amyloid goitre with thyroid aspiration biopsy. Cytopathology. 2006. 17:262–266.9. Ikenoue H, Okamura K, Kuroda T, Sato K, Yoshinari M, Fujishima M. Thyroid amyloidosis with recurrent subacute thyroiditis-like syndrome. J Clin Endocrinol Metab. 1988. 67:41–45.10. Sipe JD, Cohen AS. Review: history of the amyloid fibril. J Struct Biol. 2000. 130:88–98.11. Lachmann HJ, Goodman HJ, Gilbertson JA, Gallimore JR, Sabin CA, Gillmore JD, Hawkins PN. Natural history and outcome in systemic AA amyloidosis. N Engl J Med. 2007. 356:2361–2371.12. Akçay S, Akman B, Ozdemir H, Eyüboğlu FO, Karacan O, Ozdemir N. Bronchiectasis-related amyloidosis as a cause of chronic renal failure. Ren Fail. 2002. 24:815–823.13. Gertz MA, Kyle RA. Secondary systemic amyloidosis: response and survival in 64 patients. Medicine (Baltimore). 1991. 70:246–256.14. Kimura H, Yamashita S, Ashizawa K, Yokoyama N, Nagataki S. Thyroid dysfunction in patients with amyloid goitre. Clin Endocrinol (Oxf). 1997. 46:769–774.15. Park KY, Park KL, Han SY, Cho SR, Lee K, Kang YW, Park SB, Kim HC, Kim SP, Kwon KY. Amyloid goiter. J Korean Soc Endocrinol. 1995. 10:125–130.16. Cohan P, Hirschowitz S, Rao JY, Tanavoli S, Van Herle AJ. Amyloid goiter in a case of systemic amyloidosis secondary to ankylosing spondylitis. J Endocrinol Invest. 2000. 23:762–764.17. el-Reshaid K, al-Tamami M, Johny KV, Madda JP, Hakim A. Amyloidosis of the thyroid gland: role of ultrasonography. J Clin Ultrasound. 1994. 22:239–244.18. Rajkumar SV, Gertz MA. Advances in the treatment of amyloidosis. N Engl J Med. 2007. 356:2413–2415.19. Dember LM, Hawkins PN, Hazenberg BP, Gorevic PD, Merlini G, Butrimiene I, Livneh A, Lesnyak O, Puéchal X, Lachmann HJ, Obici L, Balshaw R, Garceau D, Hauck W, Skinner M. Eprodisate for AA Amyloidosis Trial Group. Eprodisate for the treatment of renal disease in AA amyloidosis. N Engl J Med. 2007. 356:2349–2360.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Graves' Disease Following Subacute Thyroiditis
- A case of an autonomously functioning thyroid nodule combined with subacute thyroiditis
- A Case of Riedel's Thyroiditis in a Patient with a History of Subacute Thyroiditis
- A Case of Painful Hashimoto's Thyroiditis Successfully Treated with Total Thyroidectomy
- Graves' Disease Following Recurrent Subacute Thyroiditis