Endocrinol Metab.
2012 Jun;27(2):163-168. 10.3803/EnM.2012.27.2.163.
A Case of Parathyroid Apoplexy of Primary Hyperparathyroidism Presenting as Auditory Hallucinations Accompanied with Hypocalcemia
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University Hospital, Kyungpook National University School of Medicine, Daegu, Korea. jugkim@knu.ac.kr
- KMID: 1497659
- DOI: http://doi.org/10.3803/EnM.2012.27.2.163
Abstract
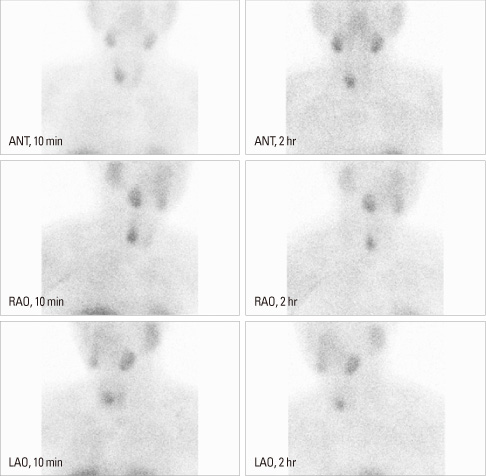
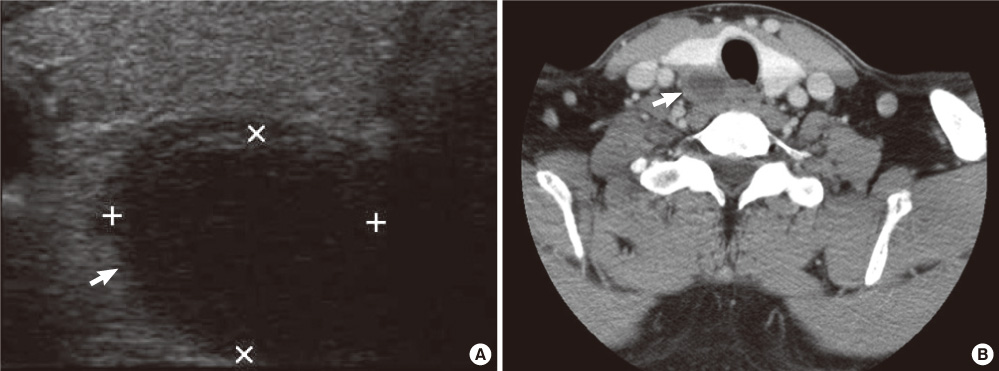
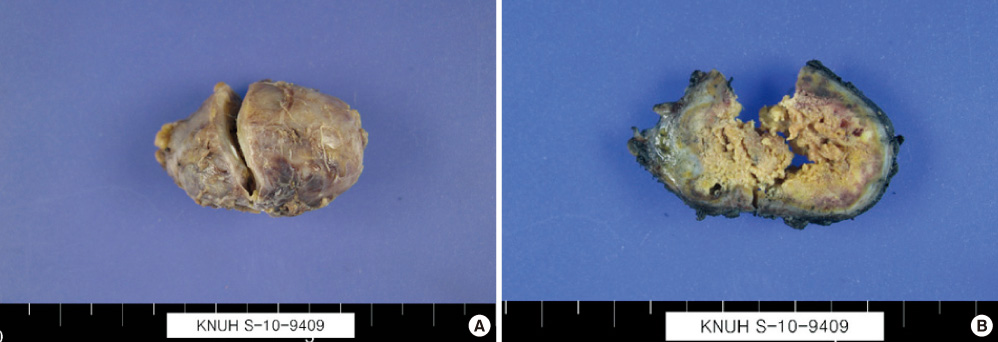
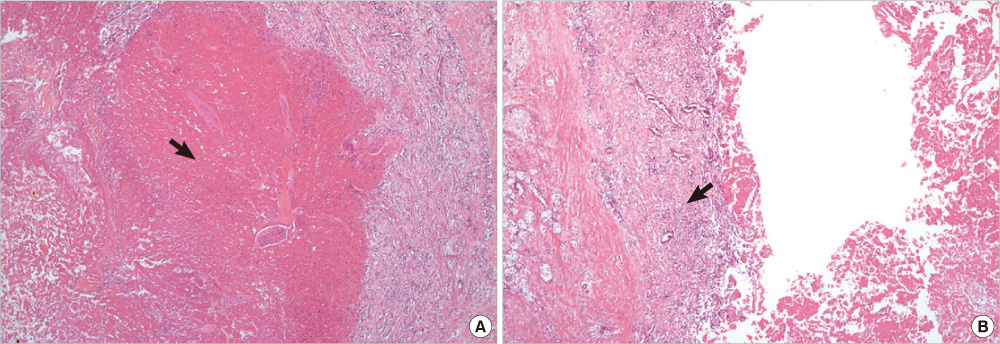
- The natural history of primary hyperparathyroidism, due to parathyroid adenoma, is unknown. Furthermore, spontaneous resolution of parathyroid necrosis or hemorrhage is rare and usually asymptomatic. Here, we report a case of parathyroid apoplexy of primary hyperparathyroidism, presenting as auditory hallucinations, accompanied with hypocalcemia. A 39-year-old man who was incidentally diagnosed with primary hyperparathyroidism, and waiting surgery for parathyroidectomy presented to psychiatric service with auditory hallucinations. He developed tetany, while taking psychiatric drugs. On a follow-up investigation, his serum calcium level fell from 11.8 to 5.8 mg/dL. His intact parathyroid hormone level also decreased from 1,017 pg/mL to 71.1 pg/mL. The parathyroid apoplexy was confirmed after a surgical removal of the infarcted adenoma. The auditory hallucinations disappeared, and serum calcium level was returned to within the normal range.
MeSH Terms
Figure
Reference
-
1. Geffken GR, Ward HE, Staab JP, Carmichael SL, Evans DL. Psychiatric morbidity in endocrine disorders. Psychiatr Clin North Am. 1998. 21:473–489.2. Feldman F, Mitchell W, Soll S. Psychosis, Cushing's syndrome and hyperparathyroidism. Can Med Assoc J. 1968. 98:508–511.3. Efremidou EI, Papageorgiou MS, Pavlidou E, Manolas KJ, Liratzopoulos N. Parathyroid apoplexy, the explanation of spontaneous remission of primary hyperparathyroidism: a case report. Cases J. 2009. 2:6399.4. Wootten CT, Orzeck EA. Spontaneous remission of primary hyperparathyroidism: a case report and meta-analysis of the literature. Head Neck. 2006. 28:81–88.5. Fraser WD. Hyperparathyroidism. Lancet. 2009. 374:145–158.6. Silverberg SJ, Shane E, Jacobs TP, Siris E, Bilezikian JP. A 10-year prospective study of primary hyperparathyroidism with or without parathyroid surgery. N Engl J Med. 1999. 341:1249–1255.7. Petersen P. Psychiatric disorders in primary hyperparathyroidism. J Clin Endocrinol Metab. 1968. 28:1491–1495.8. Cope O. Hyperparathyroidism: diagnosis and management. Am J Surg. 1960. 99:394–403.9. Joborn C, Hetta J, Palmér M, Akerström G, Ljunghall S. Psychiatric symptomatology in patients with primary hyperparathyroidism. Ups J Med Sci. 1986. 91:77–87.10. Walker MD, McMahon DJ, Inabnet WB, Lazar RM, Brown I, Vardy S, Cosman F, Silverberg SJ. Neuropsychological features in primary hyperparathyroidism: a prospective study. J Clin Endocrinol Metab. 2009. 94:1951–1958.11. Devaris DP, Mehlman I. Psychiatric presentations of endocrine and metabolic disorders. Prim Care. 1979. 6:245–265.12. Guisado R, Arieff AI, Massry SG, Lazarowitz V, Kerian A. Changes in the electroencephalogram in acute uremia. Effects of parathyroid hormone and brain electrolytes. J Clin Invest. 1975. 55:738–745.13. Bilezikian JP. Primary hyperparathyroidism. Drug Ther. 1982. 7:41–48.14. Norris EH. Primary hyperparathyroidism; a report of five cases that exemplify special features of this disease (infarction of a parathyroid adenoma; oxyphil adenoma). Arch Pathol (Chic). 1946. 42:261–273.15. Nylen E, Shah A, Hall J. Spontaneous remission of primary hyperparathyroidism from parathyroid apoplexy. J Clin Endocrinol Metab. 1996. 81:1326–1328.16. Natsui K, Tanaka K, Suda M, Yasoda A, Yonemitsu S, Nakao K. Spontaneous remission of primary hyperparathyroidism due to hemorrhagic infarction in the parathyroid adenoma. Intern Med. 1996. 35:646–649.17. Mir R, Gerold T, Khan S, Weitz J. Spontaneous infarction of parathyroid adenoma: case report and literature review. Head Neck. 1993. 15:566–568.18. Kovacs KA, Gay JD. Remission of primary hyperparathyroidism due to spontaneous infarction of a parathyroid adenoma. Case report and review of the literature. Medicine (Baltimore). 1998. 77:398–402.19. Govindaraj S, Wasserman J, Rezaee R, Pearl A, Bergman DA, Wang BY, Urken ML. Parathyroid adenoma autoinfarction: a report of a case. Head Neck. 2003. 25:695–699.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Parathyroid Adenoma without Hyperparathyroidism Presenting as a Large Neck Mass
- A Case of Primary Hyperparathyroidism Associated with Proximal Renal Tubular Acidosis and Postoperative Hungry Bone Syndrome
- A Case of Parathyroid Carcinoma Presenting as Brown Tumors
- Primary Hyperparathyroidism in Recurrent Urolithiasis: 1 Case
- Two Cases of Hungry Bone Syndrome after Huge Parathyroidectomy