Korean J Radiol.
2013 Apr;14(2):269-277. 10.3348/kjr.2013.14.2.269.
Value of 3-Dimensional CT Virtual Anatomy Imaging in Complex Foreign Body Retrieval from Soft Tissues
- Affiliations
-
- 1Department of Radiology, Shanghai Eighth People's Hospital, Shanghai 200235, China. woothingyang2008@126.com
- 2Department of General Surgery, Shanghai Eighth People's Hospital, Shanghai 200235, China.
- KMID: 1482786
- DOI: http://doi.org/10.3348/kjr.2013.14.2.269
Abstract
OBJECTIVE
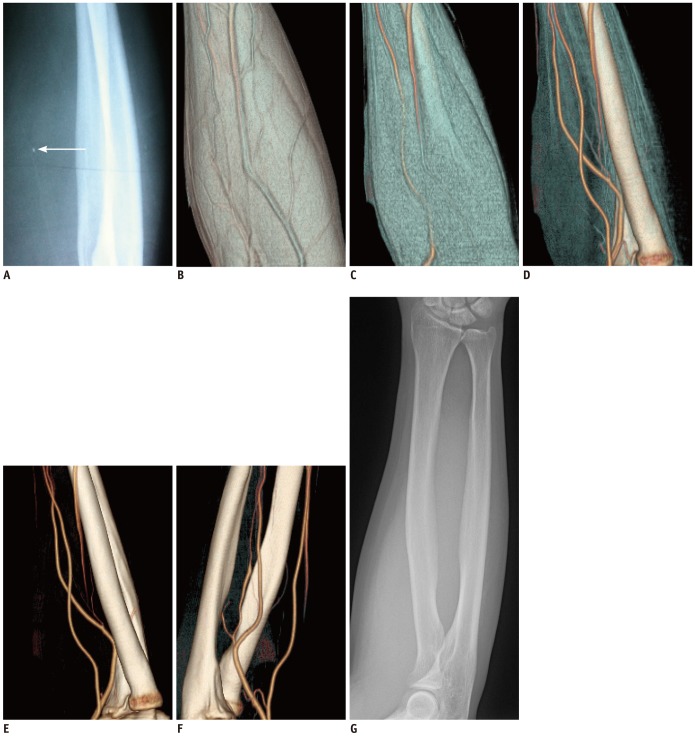
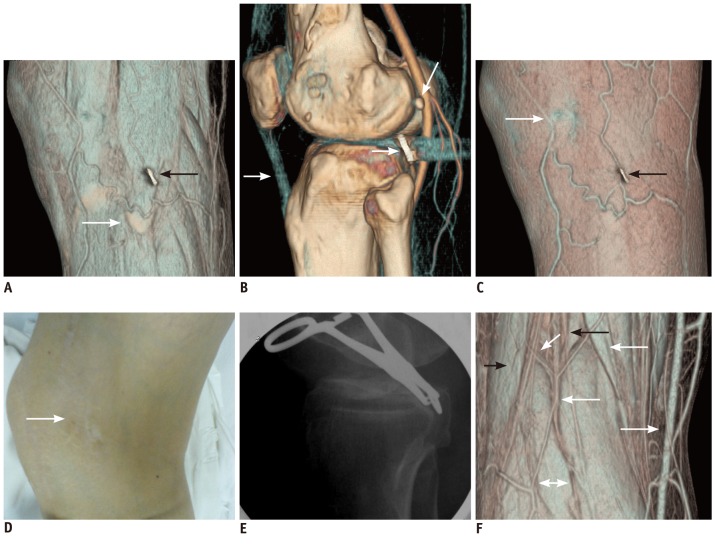
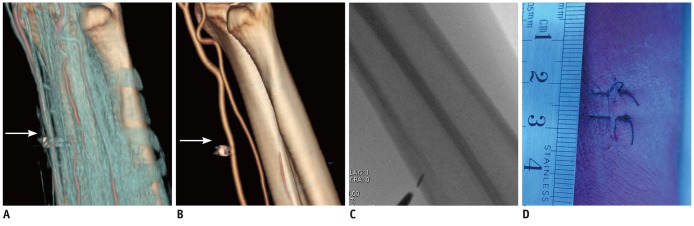
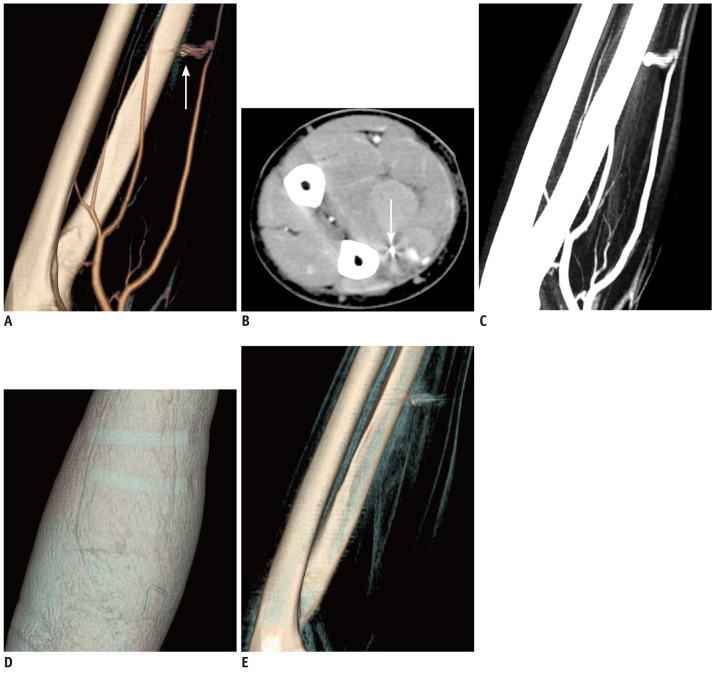
To investigate the value of 3-dimensional (3D) CT virtual anatomy imaging (VAI) in the complex foreign body (FB) retrieval of the soft tissues.
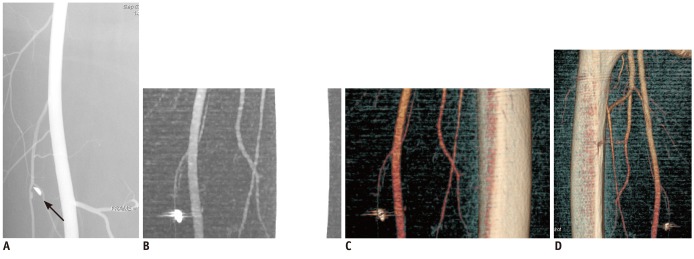
MATERIALS AND METHODS
Four hundred and seventy-five patients with radiopaque FB(s) diagnosed by radiograph underwent contrast-enhanced 3D CT examination. VAI was reconstructed by volume-rendering opacity software, by sliding down the lowest threshold from -600 to 100 HU. The imaging was grouped into three groups: A (axial and multi-planar reformation [MPR] images), B (standard 3D imaging with axial and MPR images), and C (VAI with axial and MPR images). They were analyzed to reveal the type, size, number, location, complications, and the interventional removability of the object, with the comparisons in the management and clinical outcomes on the patient follow-up studies. The data were subjected to chi-square tests, with p value < 0.05 indicating significant statistical difference.
RESULTS
The FB shape, size, number, site distribution and vessels around FB, as well as the FB-associated vascular complications and the FB interventional removability were assessed more accurately in Group C than in Group B or Group A (p < 0.005). There was no significant difference in disclosing the type and depth of the FB among the three groups (p > 0.75). On the basis of the 3D CT, especially the enhanced 3D CT VAI, the followings were processed: the recommendation of interventional removal in 286 (60.47%) and non-intervention in 187 (39.53%) of the 473 patients with soft-tissue FB(s); in 352 (56.50%) of the 623 radiopaque FBs patients, 258 (54.55%) patients accurately detected on 3D CT and the successful removal by intervention (343 FBs) or surgery (9 FBs) without any sequela; and 215 (45.45%) patients with 271 FBs lost in the follow-up, with their departure from the hospital.
CONCLUSION
The 3D CT, especially 3D enhanced CT VAI, has great incremental value in further diagnosis and management of complex FB extraction from soft tissues.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Contrast Media/diagnostic use
Female
Foreign Bodies/*radiography/surgery
Humans
*Imaging, Three-Dimensional
Iohexol/diagnostic use
Male
Middle Aged
Radiographic Image Interpretation, Computer-Assisted
Tomography, X-Ray Computed/*methods
Treatment Outcome
User-Computer Interface
Contrast Media
Iohexol
Figure
Reference
-
1. Callegari L, Leonardi A, Bini A, Sabato C, Nicotera P, Spano' E, et al. Ultrasound-guided removal of foreign bodies: personal experience. Eur Radiol. 2009; 19:1273–1279. PMID: 19153745.
Article2. Park TH, Seo SW, Kim JK, Chang CH. Clinical outcome in a series of 173 cases of foreign body granuloma: improved outcomes with a novel surgical technique. J Plast Reconstr Aesthet Surg. 2012; 65:29–34. PMID: 21885359.
Article3. Ando A, Hatori M, Hagiwara Y, Isefuku S, Itoi E. Imaging features of foreign body granuloma in the lower extremities mimicking a soft tissue neoplasm. Ups J Med Sci. 2009; 114:46–51. PMID: 19242872.
Article4. Nocturne G, Sellam J, Miquel A, M'Bappé P, Berenbaum F. Is sarcoma a complication of arterial femoro-popliteal bypass? Joint Bone Spine. 2010; 77:358–360. PMID: 20471894.
Article5. Hunter TB, Taljanovic MS. Foreign bodies. Radiographics. 2003; 23:731–757. PMID: 12740473.
Article6. Young AS, Shiels WE 2nd, Murakami JW, Coley BD, Hogan MJ. Self-embedding behavior: radiologic management of self-inserted soft-tissue foreign bodies. Radiology. 2010; 257:233–239. PMID: 20823372.
Article7. Lammers RL. Soft tissue foreign bodies. Ann Emerg Med. 1988; 17:1336–1347. PMID: 3057951.
Article8. Lammers RL, Magill T. Detection and management of foreign bodies in soft tissue. Emerg Med Clin North Am. 1992; 10:767–781. PMID: 1425403.
Article9. Bakshi J, Verma RK, Karuppiah S. Migratory foreign body of neck in a battered baby: a case report. Int J Pediatr Otorhinolaryngol. 2009; 73:1814–1816. PMID: 19879659.
Article10. Croy T. Metallic foreign body in a patient with knee pain. J Orthop Sports Phys Ther. 2011; 41:696. PMID: 21885912.
Article11. Hecht S, Adams WH, Narak J, Thomas WB. Magnetic resonance imaging susceptibility artifacts due to metallic foreign bodies. Vet Radiol Ultrasound. 2011; 52:409–414. PMID: 21382122.
Article12. Kiliç A, Avcu S, Tekïn S, Gül A, Cïnal A, Yasar T. MRI-Induced Migration of Retained Metallic Foreign Body in the Eye. Ophthalmic Surg Lasers Imaging. 2010; 1–3.
Article13. Sun Z. 3D multislice CT angiography in post-aortic stent grafting: a pictorial essay. Korean J Radiol. 2006; 7:205–211. PMID: 16969051.
Article14. Meurer WJ. Radial artery pseudoaneurysm caused by occult retained glass from a hand laceration. Pediatr Emerg Care. 2009; 25:255–257. PMID: 19369839.
Article15. Tao K, Xu S, Liu XY, Liang JL, Qiu T, Tan JN, et al. Small metal soft tissue foreign body extraction by using 3D CT guidance: a reliable method. Eur J Radiol. 2012; 81:3339–3343. PMID: 22321905.
Article16. Nemsadze G, Urushadze O. The role of multislice spiral computed tomography in the diagnosis and management of acute facial trauma in patients with multiple injuries. Georgian Med News. 2011; 11:36–42. PMID: 22201078.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Virtual Endoscopy of Impacted Foreign Bodies in Tracheal and Esophageal Model
- The Utility of Three-dimensional CT in Orbital Diseases
- Percutaneous Retrieval of a Migrated Surgical Drainage Tube in the Chest Wall with the Nitinol Goose Neck Snare
- Usefulness of Two-dimensioanl CT & Three-dimensional CT in Blow-out Fracture
- MDCT Application of Thoracic Imaging