J Cardiovasc Ultrasound.
2009 Mar;17(1):10-15. 10.4250/jcu.2009.17.1.10.
Correlation between Stroke and Spontaneous Echo Contrast by Tissue Harmonic Imaging in Patients with Dilated Cardiomyopathy
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. dgpark@hallym.or.kr
- KMID: 1473761
- DOI: http://doi.org/10.4250/jcu.2009.17.1.10
Abstract
- BACKGROUND
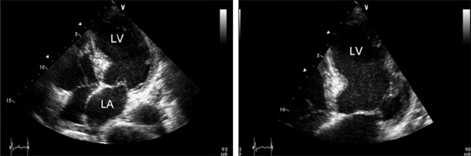
Spontaneous echo contrast (SEC) has been considered as a predisposition to thromboembolism and cerebrovascular accident. However, there have been few reports on the prevalence and role of SEC in dilated cardiomyopathy (DCM). The aim of this study was to investigate the prognostic usefulness of SEC in predicting a stroke in patients with DCM.
METHODS
Between October 2001 and January 2008, transthoracic echocardiography with tissue harmonic imaging (THI) was performed for recognition of SEC in patients with DCM. Patients were divided into 2 groups according to the presence of SEC. Clinical characteristic data, echocardiographic parameters were compared between two groups.
RESULTS
In this retrospective study, 220 patients (136 men, age 62.8+/-15.4 years) with DCM (left ventricular ejection fraction 27.8+/-7.8%) were included. SEC in the left ventricle (LV) was observed in 24 patients (10.9%). Stroke occurred in 4 (16.7%) of patients with SEC and in 9 (4.6%) of patients without SEC. There were no differences in LA dimension (p=0.24) and LV end-diastolic dimension (p=0.88) between both groups. On univariate analysis, SEC and coronary heart disease at presentation had statistical significance of risk factors for stroke in these groups (p<0.05). On multivariate analysis, only SEC was an independent predictor for stroke (OR 4.393, 95% CI 1.116-17.290, p=0.03).
CONCLUSION
These results suggest that SEC by THI through transthoracic echocardiography has a strong association with stroke in patients with DCM. Therefore, this study may help in the risk stratification of cardiac embolism in patients with DCM.
MeSH Terms
Figure
Reference
-
1. Chimowitz MI, DeGeorgia MA, Poole RM, Hepner A, Armstrong WM. Left atrial spontaneous echo contrast is highly associated with previous stroke in patients with atrial fibrillation or mitral stenosis. Stroke. 1993. 24:1015–1019.
Article2. Fatkin D, Kelly RP, Feneley MP. Relations between left atrial appendage blood flow velocity, spontaneous echocardiographic contrast and thromboembolic risk in vivo. J Am Coll Cardiol. 1994. 23:961–969.
Article3. Zotz RJ, Müller M, Genth-Zotz S, Darius H. Spontaneous echo contrast caused by platelet and leukocyte aggregates? Stroke. 2001. 32:1127–1133.
Article4. Feigenbaum H. Coronary artery disease. Echocardiography. 1975. 2nd ed. Philadelphia: Lea and Febiger;341–380.5. Castello R, Pearson AC, Labovitz AJ. Prevalence and clinical implications of atrial spontaneous contrast in patients undergoing transesophageal echocardiography. Am J Cardiol. 1990. 65:1149–1153.
Article6. Fatkin D, Herbert E, Feneley MP. Hematologic correlates of spontaneous echo contrast in patients with atrial fibrillation and implications for thromboembolic risk. Am J Cardiol. 1994. 73:672–676.
Article7. Song WH, Lim HE, Shin SH, Lee EM, Hwang KS, Ahn JC, Lim DS, Park CG, Shim WJ, Oh DJ, Ro YM. Changes of mitral inflow according to position in patients with dilated cardiomyopathy. J Korean Soc Echocardiogr. 1998. 6:5–10.
Article8. Youn HJ. Unusual form of cardiomyopathy. J Korean Soc Echocardiogr. 2005. 13:51–65.
Article9. Visser CA, Kan G, David GK, Lie KI, Durer D. Two dimensional echocardiography in the diagnosis of left ventricular thrombus: a prospective study of 67 patients with anatomic validation. Chest. 1983. 83:228–232.
Article10. Arvan S. Mural thrombi in coronary artery disease: recent advances in pathogenesis, diagnosis, and approaches to treatment. Arch Intern Med. 1984. 144:113–116.
Article11. Shaw LJ. Impact of contrast echocardiography on diagnostic algorithms: pharmacoeconomic implications. Clin Cardiol. 1997. 20:I39–I48.
Article12. Thomas JD, Rubin DN. Tissue harmonic imaging: why does it work? J Am Soc Echocardiogr. 1998. 11:803–808.
Article13. Rubin DN, Yazbek N, Garcia MJ, Stewart WJ, Thomas JD. Qualitative and quantitative effects of harmonic echocardiographic imaging on endocardial edge definition and side-lobe artifacts. J Am Soc Echocardiogr. 2000. 13:1012–1018.
Article14. Mele D, Campana M, Sclavo M, Seveso G, Aschieri D, Nesta F, D'Aiello I, Ferrari R, Levine RA. Impact of tissue harmonic imaging in patients with distorted left ventricles: improvement in accuracy and reproducibility of visual, manual and automated echocardiographic assessment of left ventricular ejection fraction. Eur J Echocardiogr. 2003. 4:59–67.
Article15. Mele D, Teoli R, Cittanti C, Pasanisi G, Guardigli G, Levine RA, Ferrari R. Assessment of left ventricular volume and function by integration of simplified 3D echocardiography, tissue harmonic imaging and automated extraction of endocardial borders. Int J Cardiovasc Imaging. 2004. 20:191–202.
Article16. Ono M, Asanuma T, Tanabe K, Yoshitomi H, Shimizu H, Ohta Y, Shimada T. Improved visualization of the left atrial appendage by transthoracic 2-dimensional tissue harmonic compared with fundamental echocardiographic imaging. J Am Soc Echocardiogr. 1998. 11:1044–1049.
Article17. Mele D, Soukhomovskaia O, Pacchioni E, Merli E, Avigni N, Federici L, Levine R, Ferrari R. Improved detection of left ventricular thrombi and spontaneous echocontrast by tissue harmonic imaging in patients with myocardial infarction. J Am Soc Echocardiogr. 2006. 19:1373–1381.
Article18. Meltzer RS, Visser CA, Fuster V. Intracardiac thrombi and systemic immobilization. Ann Intern Med. 1986. 104:689–698.19. Kidwell CS, Warach S. Acute ischemic cerebrovascular syndrome: diagnostic criteria. Stroke. 2003. 34:2995–2998.20. Sharma ND, McCullough PA, Philbin EF, Weaver WD. Left ventricular thrombus and subsequent thromboembolism in patients with severe systolic dysfunction. Chest. 2000. 117:314–320.
Article21. Richardson P, McKenna W, Bristow M, Maisch B, Mauter B, O'connell J, Olsen E, Thiene G, Goodwin J, Gyarfas I, Martin I, Nordet P. Report of the 1995 World health organization/international society and federation of cardiology task force on the definition and classification of cardiomyopathies. Circulation. 1996. 93:841–842.
Article22. Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978. 58:1072–1083.
Article23. Gottdiener JS, Gay JA, Van Voorhees L, DiBianco R, Fletcher RD. Frequency and embolic potential of left ventricular thrombus in dilated cardiomyopathy: assessment by 2-dimensional echocardiography. Am J Cardiol. 1983. 52:1281–1285.
Article24. Fuster V, Halperin JL. Left ventricular thrombi and cerebral embolism. N Engl J Med. 1989. 320:392–394.
Article25. Kozdag G, Ciftci E, Vural A, Selekler M, Sahin T, Ural D, Kahraman G, Agacdiken A, Demirci A, Komsuoglu S, Komsuoglu B, Fici F. Silent cerebral infarction in patients with dilated cardio-myopathy: echocardiographic correlates. Int J Cardiol. 2006. 107:376–381.
Article26. Falk RH, Foster E, Coats MH. Ventricular thrombi and thromboembolism in dilated cardiomyopathy: a prospective follow-up study. Am Heart J. 1992. 123:136–142.
Article27. Hunt SA, Baker DW, Chin HM, Cinquegrani MP, Feldman AM, Francis GS, Ganiats TG, Goldstein S, Gregoratos G, Jessup ML, Noble RJ, Packer M, Silver MA, Stevenson LW, Gibbons RJ, Antman EM, Alpert JS, Faxon DP, Fuster V, Jacobs AK, Hiratzka LF, Russell RO, Smith SC Jr. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary a report of the American college of cardiology/American heart association task force on practice guidelines (committee to revise the 1995 guidelines for the evaluation and management of heart failure): developed in collaboration with the international society for heart and lung transplantation: endorsed by the heart failure society of America. Circulation. 2001. 104:2996–3007.
Article28. Ansari A, Maron BJ. Spontaneous echo contrast and thromboembolism. Hosp Pract (Minneap). 1997. 32:109–111. 115–116.
Article29. Belohlavek M, Tanabe K, Mulvagh SL, Foley DA, Greenleaf JF, Seward JB. Image enhancement by noncontrast harmonic echocardiography: part II. Quantitative assessment with use of contrast-to-speckle. Mayo Clin Proc. 1998. 73:1066–1070.
Article30. Main ML, Asher CR, Rubin DN, Odabashian JA, Cardon LA, Thomas JD, Klein AL. Comparison of tissue harmonic imaging with contrast (sonicated albumin) echocardiography and Doppler myocardial imaging for enhancing endocardial border resolution. Am J Cardiol. 1999. 83:218–222.
Article31. Hwang JH, Yang DH, Shin SC, Cho S, Kim TI, Park HS, Cho YK, Chae SC, Jun JE, Park WH. Value of tissue harmonic imaging for the left ventricular wall imaging. J Kor Soc Echocardiogr. 2000. 8:198–205.
Article32. Ha JW, Chung N, Kang SM, Jang KJ, Kim IJ, Rim SJ, Jang Y, Shim WH, Cho SY, Kim SS. Enhanced detection of left atrial spontaneous echo contrast by transthoracic harmonic imaging in mitral stenosis. J Am Soc Echocardiogr. 2000. 13:849–854.
Article33. Daniel WG, Nellessen U, Schroder E, Nonnast-Daniel B, Bednarski P, Nikutta P, Lichtlen PR. Left atrial spontaneous echo contrast in mitral valve disease: an indicator for an increased thromboembolic risk. J Am Coll Cardiol. 1988. 11:1204–1211.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cerebral Thromboembolism Occurred after Restoration to Sinus Rhythm of Paroxysmal Atrial Flutter in Apical Hypertropic Cardiomyopathy with Spontaneous Echo Contrast(SEC)
- Enhanced Detection of Left Atrial Spontaneous Echo Contrast by Transthoracic Harmonic Imaging in Mitral Stenosis
- Hemodynamics and Left Ventricular Cineangiographic Findings in Idiopathic Dilated Cardiomyopathy
- Peak Myocardial Velocity by Tissue Doppler Imaging in the Children with Myocarditis and Dilated Cardiomyopathy
- Transesophageal Echocardiographic Findings in Stroke Subtypes