Distal Tibia Fracture: Plate Osteosynthesis
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonnam National University Medical School and Hospital, Gwangju, Korea. kbleeos@chonnam.ac.kr
- KMID: 1470001
- DOI: http://doi.org/10.12671/jkfs.2009.22.4.306
Abstract
- No abstract available.
MeSH Terms
Figure
Cited by 5 articles
-
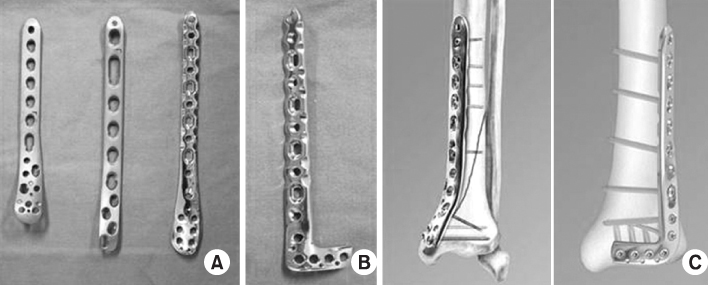
Minimally Invasive Osteosynthesis with Locking Compression Plate for Distal Tibia Fractures
Sung-Kyu Kim, Keun-Bae Lee, Keun-Young Lim, Eun-Sun Moon
J Korean Fract Soc. 2011;24(1):33-40. doi: 10.12671/jkfs.2011.24.1.33.The Result of Using an Additional Mini-Locking Plate for Tibial Pilon Fractures
Suenghwan Jo, Jun Young Lee, Boseon Kim, Kang Hyeon Ryu
J Korean Fract Soc. 2017;30(2):75-82. doi: 10.12671/jkfs.2017.30.2.75.Management of Fractures of Distal Tibia by Minimally Invasive Plate Osteosynthesis through an Anterior Approach
Gu-Hee Jung, Jae-Do Kim, Jae-Ho Jang, Sung-Keun Heo, Dong-won Lee
J Korean Orthop Assoc. 2010;45(6):473-481. doi: 10.4055/jkoa.2010.45.6.473.Anterolateral Minimally Invasive Plate Osteosynthesis of Distal Tibial Fractures Using an Anterolateral Locking Plate
Dongwhan Suh, Hwan Hee Lee, Young Hoon Han, Jae Jung Jeong
J Korean Foot Ankle Soc. 2020;24(1):19-24. doi: 10.14193/jkfas.2020.24.1.19.Minimally Invasive Plate Osteosynthesis for Fractures of Distal Tibia
Tae Hun Kim, So Hak Chung
Kosin Med J. 2014;29(1):23-29. doi: 10.7180/kmj.2014.29.1.23.
Reference
-
1. Arens S, Kraft C, Schleqel U, Printzen G, Perren SM, Hansis M. Susceptibility to local infection in biological internal fixation. Experimental study of open vs minimally plate osteosynthesis in rabbits. Arch Orthop Trauma Surg. 1999; 119:82–85.2. Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. J Am Acad Orthop Surg. 2006; 14:406–416.
Article3. Borg T, Larsson S, Lindsjö U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury. 2004; 35:608–614.4. Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res. 2000; 375:69–77.
Article5. Foux A, Yeadon AJ, Uhthoff HK. Improved fracture healing with less rigid plates. A biomechanical study in dogs. Clin Orthop Relat Res. 1997; 339:232–245.
Article6. Francois J, Vandeputte G, Verheyden F, Nelen G. Percutaneous plate fixation of fractures of the distal tibia. Acta Orthop Belg. 2004; 70:148–154.7. Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007; 38:365–370.
Article8. Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia-results in 20 patients. Injury. 2006; 37:877–887.
Article9. Helfet DL, Shonnard PY, Levine D, Borrelli J Jr. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997; 28:A42–A47.
Article10. Helfet DL, Suk M. Minimally invasive percutaneous plate osteosynthesis of fractures of the distal tibia. Instr Course Lect. 2004; 53:471–475.11. Krackhardt T, Dilger J, Flesch I, Höntzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg. 2005; 125:87–94.
Article12. Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2008; 32:697–703.
Article13. Maffulli N, Toms AD, McMurtie A, Olive F. Percutaneous plating of distal tibial fractures. Int Orthop. 2004; 28:159–162.
Article14. Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res. 2003; 408:286–291.
Article15. Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury. 2004; 35:615–620.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of distal tibia metaphyseal fractures by percutaneous plate osteosynthesis
- Clinical Outcomes of Locking Compression Plate Fixation through Minimally Invasive Percutaneous Plate Osteosynthesis in the Treatment of Distal Tibia Fracture
- Analysis of the Result Treated with Locking Compression Plate-Distal Tibia and Zimmer Periarticular Locking Plate in Distal Tibia Fracture
- Minimally Invasive Percutaneous Plate Osteosynthesis Using Periarticular Plate for Distal Tibial Fractures
- Surgical Treatment of Distal Tibia Fractures