J Korean Surg Soc.
2009 Apr;76(4):252-258. 10.4174/jkss.2009.76.4.252.
Analysis of the Management of Children with Abdominal Solid Organ Injuries
- Affiliations
-
- 1Department of Surgery, Ewha Womans University School of Medicine, Seoul, Korea. kumchoi@ewha.ac.kr
- KMID: 1465064
- DOI: http://doi.org/10.4174/jkss.2009.76.4.252
Abstract
-
PURPOSE: In pediatric solid organ injury, non-operative management is considered as a standard treatment when the patient is hemodynamically stable. However, treatment according to the injured organ and the depth of injury is controversial. The purpose of this study is to evaluate treatment results in the management of abdominal solid organ injuries in children.
METHODS
This analysis was performed retrospectively with 57 consecutive children under 15 year of age who were diagnosed with abdominal solid organ injuries at Ewha Womans University Mokdong Hospital from January, 1999 to June, 2007.
RESULTS
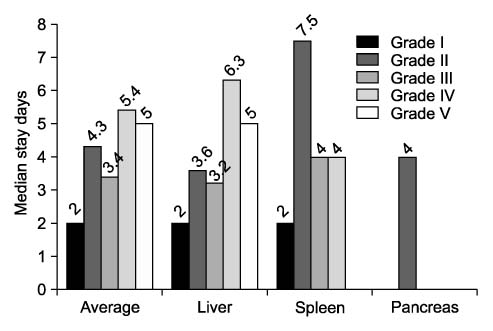
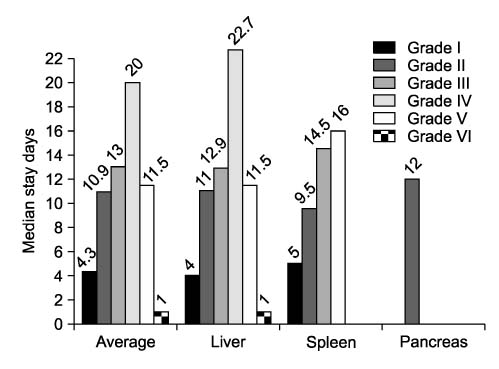
The major cause of pediatric solid organ injury was traffic accidents (59.6%) and the most frequently injured organ was the liver (66.7%). 54 patients (94.7%) were treated non-operatively and the success rate was 100%. There was no difference in type of management and success rate according to the depth of injury or the injured organs. The average ICU stay was 4.3 days, and the average hospital stay was 13.6 days and that was extended depending on the depth of injury. And according to the cause of injury, cases by traffic accident stayed significantly longer than cases by other causes.
CONCLUSION
High grade of injury is not contraindication of nonoperative management in pediatric solid organ injury. Hemodynamic instability is the only absolute indication of operation. Therefore, if the patient is stable, non-operative management with intensive observation is the choice of treatment.
Keyword
Figure
Reference
-
1. Korean National Statistical Office. Annual Report on the Cause of Death Statistics. 2006.2. Stylianos S, Pearl RH. Grosfeld JL, O'Neill JA, Fonkalsrud EW, Coran AG, editors. Abdominal trauma. Pediatric Surgery. 2006. 6th ed. Philadelphia: Mosby-Elsevier;295–316.3. Tataria M, Nance ML, Holmes JH 4th, Miller CC 3rd, Mattix KD, Brown RL, et al. Pediatric blunt abdominal injury: age is irrelevant and delayed operation is not detrimental. J Trauma. 2007. 63:608–614.4. Bond SJ, Eichelberger MR, Gotschall CS, Sivit CJ, Randolph JG. Nonoperative management of blunt hepatic and splenic injury in children. Ann Surg. 1996. 223:286–289.5. Jobst MA, Canty TG Sr, Lynch FP. Management of pancreatic injury in pediatric blunt abdominal trauma. J Pediatr Surg. 1999. 34:818–823.6. Nance ML, Lutz N, Carr MC, Canning DA, Stafford PW. Blunt renal injuries in children can be managed nonoperatively: outcome in a consecutive series of patients. J Trauma. 2004. 57:474–478.7. Stylianos S. Outcomes from pediatric solid organ injury: role of standardized care guidelines. Curr Opin Pediatr. 2005. 17:402–406.8. Mattix KD, Tataria M, Holmes J, Kristoffersen K, Brown R, Groner J, et al. Pediatric pancreatic trauma: predictors of nonoperative management failure and associated outcomes. J Pediatr Surg. 2007. 42:340–344.9. Stylianos S. The APSA Trauma Committee. Evidence-based guidelines for resource utilization in children with isolated spleen or liver injury. J Pediatr Surg. 2000. 35:164–167.10. Lee DS, Lee SC, Shin IS, Hong KC, Park HG. Abdominal trauma in childhood. J Korean Surg Soc. 1990. 38:663–670.11. Levy JL Jr, Linder LH. Major abdominal trauma in children. Am J Surg. 1970. 120:55–58.12. Jeon IS, Yoo SY, Kim SW. Clinical analysis of blunt abdominal trauma in childhood. J Korean Surg Soc. 1984. 27:576–586.13. Holmes JF, Sokolove PE, Brant WE, Palchak MJ, Vance CW, Owings JT, et al. Identification of children with intra-abdominal injuries after blunt trauma. Ann Emerg Med. 2002. 39:500–509.14. Choi KJ. Abdominal injury by falls from a height in children. J Korean Assoc Pediatr Surg. 2005. 11:115–122.15. Bivins BA, Zona JZ, Belin RP. Diagnostic peritoneal lavage in pediatric trauma. J Trauma. 1976. 16:739–742.16. Ong AW, McKenney MG, McKenney KA, Brown M, Namias N, MaCloud J, et al. Predicting the need for laparotomy in pediatric trauma patients on the basis of the ultrasound score. J Trauma. 2003. 54:503–508.17. Tas F, Ceran C, Atalar MH, Bulut S, Selbes B, Isik AO. The efficacy of ultrasonography in hemodynamically stable children with blunt abdominal trauma: a prospective comparison with computed tomography. Eur J Radiol. 2004. 51:91–96.18. Thorelius L. Emergency real-time contrast-enhanced ultrasonography for detection of solid organ injuries. Eur Radiol. 2007. 17:Suppl 6. F107–F111.19. Wegner S, Colletti JE, Van Wie D. Pediatric blunt abdominal trauma. Pediatr Clin North Am. 2006. 53:243–256.20. Miller K, Kou D, Sivit C, Stallion A, Dudgeon DL, Grisoni ER. Pediatric hepatic trauma: does clinical course support intensive care unit stay? J Pediatr Surg. 1998. 33:1459–1462.21. Isaacman DJ, Scarfone RJ, Kost SI, Gochman RF, Davis HW, Bernardo LM, et al. Utility of routine laboratory testing for detecting intra-abdominal injury in the pediatric trauma patient. Pediatrics. 1993. 92:691–694.22. Puranik SR, Hayes JS, Long J, Mata M. Liver enzymes as predictors of liver damage due to blunt abdominal trauma in children. South Med J. 2002. 95:203–206.23. Partrick DA, Bensard DD, Moore EE, Karrer FM. Nonoperative management of solid organ injuries in children results in decreased blood utilization. J Pediatr Surg. 1999. 34:1695–1699.24. Stylianos S. Compliance with evidence-based guidelines in children with isolated spleen or liver injury: a prospective study. J Pediatr Surg. 2002. 37:453–456.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful nonoperative management of a simultaneous high-grade splenic injury and devascularized kidney in Australia: a case report
- Clinical Role of Interventional Radiology in Abdominal Solid Organ Trauma
- Differential diagnosis of abdominal masses in children
- Nonoperative Management of Children with Blunt Abdominal Trauma
- Multidetector CT Findings of Solid Organ Injury Based on 2018 Updated American Association for the Surgery of Trauma Organ Injury Scaling System